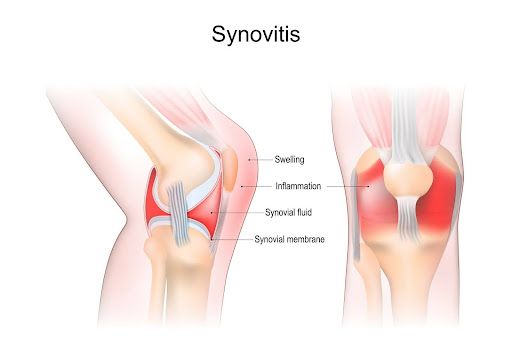
Synovitis refers to the inflammation of the synovial membrane, a specialized connective tissue lining the inner surface of joints and tendon sheaths. This condition results in excess synovial fluid production, leading to joint swelling, pain, stiffness, and reduced mobility. Synovitis can be an isolated pathology or a manifestation of systemic autoimmune disorders.
Most commonly, it affects joints such as the knee, hip, shoulder, and wrist and is frequently observed in inflammatory conditions like rheumatoid arthritis, lupus, and gout, as well as after trauma or repetitive strain.
Anatomy of the Synovial Membrane
The synovial membrane plays a critical role in joint homeostasis by producing synovial fluid, which lubricates and nourishes articular cartilage. It consists of two layers:
- Intimal Layer: Contains synoviocytes responsible for synovial fluid secretion.
- Subintimal Layer: Rich in blood vessels, lymphatics, and immune cells.
When inflamed, this structure thickens, resulting in the clinical features of synovitis.
Causes and Risk Factors of Synovitis
Synovitis arises from various etiologies, categorized broadly as:
1. Autoimmune Conditions
- Rheumatoid arthritis
- Systemic lupus erythematosus
- Psoriatic arthritis
These diseases involve immune-mediated attacks on synovial tissues, leading to chronic inflammation and joint damage.
2. Infectious Synovitis
- Septic arthritis due to bacterial invasion (e.g., Staphylococcus aureus)
- Viral arthritis in diseases like hepatitis or HIV
Prompt diagnosis is essential due to the risk of irreversible joint destruction.
3. Crystal-Induced Synovitis
- Gout (uric acid crystals)
- Pseudogout (calcium pyrophosphate crystals)
These conditions provoke acute and intensely painful flares.
4. Traumatic or Overuse Injuries
- Post-injury synovitis from ligament tears or cartilage damage
- Repetitive motion injuries in athletes
5. Degenerative Joint Disease
- Osteoarthritis may lead to secondary synovial inflammation, particularly in weight-bearing joints.
Common Symptoms of Synovitis
The clinical presentation varies based on the underlying cause and severity, but frequently includes:
- Swollen joints with a palpable effusion
- Pain that worsens with movement
- Stiffness, particularly in the morning or after periods of rest
- Warmth and redness over the affected joint
- Restricted joint mobility
In chronic cases, symptoms may persist for months and lead to joint deformity if untreated.
Diagnostic Methods for Synovitis
1. Clinical Examination
- Palpation for tenderness and swelling
- Assessment of joint range of motion and function
2. Imaging Studies
- Ultrasound: Detects fluid accumulation and synovial thickening
- MRI: Provides detailed evaluation of synovial proliferation and joint integrity
- X-rays: Useful in chronic cases to identify joint space narrowing or erosions
3. Laboratory Investigations
- Blood tests for inflammatory markers (ESR, CRP)
- Autoantibody screening: Rheumatoid factor, anti-CCP, ANA
- Synovial fluid analysis: Assesses white cell count, crystals, and potential infection
Types of Synovitis
| Type | Description | Commonly Associated Conditions |
|---|---|---|
| Acute Synovitis | Rapid onset, often painful and swollen joint | Gout, trauma |
| Chronic Synovitis | Persistent inflammation with synovial hypertrophy | Rheumatoid arthritis, lupus |
| Villonodular Synovitis | Pigmented villonodular synovitis (PVNS), a benign proliferative disorder | Idiopathic |
| Transient Synovitis | Self-limiting inflammation, particularly in children | Post-viral |
| Infectious Synovitis | Due to direct infection | Septic arthritis |
Treatment Options for Synovitis
Management is determined by the underlying cause, duration, and joint involved.
1. Medications
- NSAIDs (e.g., ibuprofen, naproxen) to reduce pain and inflammation
- Corticosteroids: Oral or intra-articular injections for severe inflammation
- DMARDs (Disease-Modifying Anti-Rheumatic Drugs) like methotrexate for autoimmune synovitis
- Biologics (e.g., TNF inhibitors) in refractory rheumatoid synovitis
2. Aspiration and Synovial Fluid Analysis
- Reduces pressure and confirms diagnosis
3. Surgical Intervention
- Synovectomy (surgical removal of inflamed synovium) in chronic or recurrent cases
- Arthroscopic or open approaches depending on joint and severity
4. Physical Therapy
- Maintains joint mobility
- Prevents stiffness and muscle atrophy
5. Lifestyle Modifications
- Weight loss for joint offloading
- Joint protection techniques in daily activities
Complications of Untreated Synovitis
- Cartilage degradation
- Joint deformity and ankylosis
- Osteoporosis due to inactivity
- Reduced quality of life from chronic pain
Prompt intervention is key to preventing permanent disability.
Synovitis in Specific Joints
Knee Synovitis
The most commonly affected joint. Symptoms include joint locking, giving way, and crepitus. Often seen in athletes, post-traumatic arthritis, and systemic inflammatory conditions.
Hip Synovitis
Includes transient synovitis in children—a self-limiting cause of hip pain—or chronic cases from inflammatory diseases. MRI is vital due to deep joint location.
Shoulder and Wrist Synovitis
May present with minimal swelling but marked dysfunction. Seen in rheumatoid arthritis and repetitive strain injuries.
Preventive Strategies
While not all forms of synovitis are preventable, especially those related to autoimmune disorders, the following steps can reduce risk:
- Regular joint-friendly exercise (e.g., swimming, walking)
- Early treatment of infections and injuries
- Adequate hydration and uric acid control in gout
- Monitoring autoimmune disease activity
- Ergonomic practices for repetitive-motion occupations
Frequently Asked Questions:
Q1. Is synovitis a permanent condition?
Not necessarily. Acute synovitis may resolve with treatment, while chronic forms require ongoing management.
Q2. Can synovitis go away on its own?
Mild or transient cases, especially in children, can resolve spontaneously. Persistent inflammation needs medical attention.
Q3. What is the best treatment for synovitis?
Treatment depends on the cause. NSAIDs, corticosteroids, or DMARDs are commonly used, and physical therapy aids recovery.
Q4. How is synovitis different from arthritis?
Synovitis is inflammation of the synovial membrane, while arthritis refers broadly to joint inflammation, which may or may not involve synovitis.
Q5. Is synovitis serious?
If left untreated, it can lead to permanent joint damage. Timely diagnosis and appropriate therapy are essential.