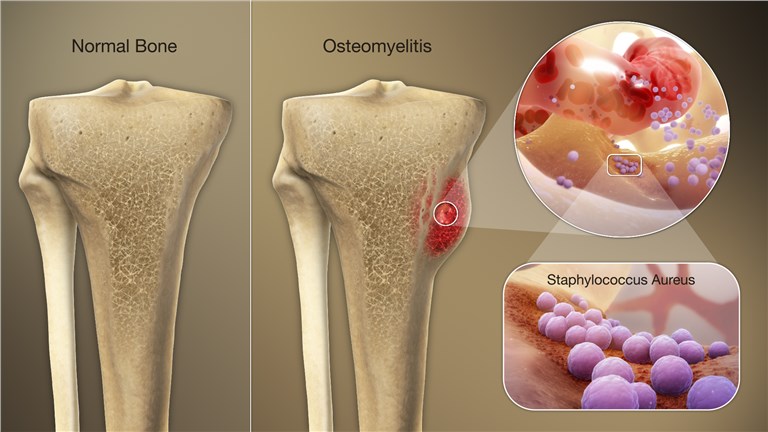
Staphylococcal osteomyelitis, particularly that caused by Staphylococcus aureus, remains a significant therapeutic challenge due to its ability to invade bone tissue, form biofilms, and persist within osteoblasts. Methicillin-resistant S. aureus (MRSA) poses an even greater hurdle, requiring advanced treatment strategies. The use of synergistic antibiotic combinations has emerged as a critical tool in enhancing treatment efficacy, reducing resistance, and improving long-term outcomes.
Mechanism and Rationale for Antibiotic Synergy
Antibiotic synergy occurs when the combined effect of two or more agents exceeds the sum of their independent effects. In osteomyelitis, where bacteria reside in poorly vascularized bone and within biofilms, monotherapy often fails to penetrate and eradicate infection. Synergistic combinations improve antimicrobial action by:
- Disrupting biofilm integrity and bacterial adhesion
- Enhancing intracellular penetration and bone affinity
- Lowering the emergence of resistant subpopulations
- Producing bactericidal effects at lower doses
Core Synergistic Combinations in Osteomyelitis Treatment
Rifampin-Based Regimens for Biofilm and Intracellular Activity
Rifampin exhibits excellent biofilm penetration and intracellular bactericidal activity. However, resistance develops rapidly if used as monotherapy. Therefore, rifampin is always administered in combination with other agents.
Common regimens:
- Rifampin + Vancomycin: Synergistic against MRSA osteomyelitis, particularly in cases involving orthopedic hardware.
- Rifampin + Daptomycin: Demonstrated superior bactericidal activity in deep-seated infections and biofilms.
- Rifampin + Fluoroquinolones (e.g., Levofloxacin or Moxifloxacin): Effective against MSSA in chronic osteomyelitis and prosthetic infections.
Vancomycin Combination Therapy
Vancomycin is often the first-line agent for MRSA osteomyelitis. Its synergy with beta-lactams and other agents significantly boosts its efficacy.
- Vancomycin + Ceftaroline: Dual action on the bacterial cell wall and proven synergy in persistent MRSA infections.
- Vancomycin + Piperacillin-Tazobactam: Shown to improve bactericidal activity in selected cases.
- Vancomycin + Rifampin: Reduces relapse in hardware-associated bone infections.
Synergy in Treating Chronic and Refractory Osteomyelitis
Chronic osteomyelitis often involves mature biofilms, necrotic bone, and dormant bacterial populations. These factors contribute to recurrence and treatment failure.
Key Combination Strategies:
- Linezolid + Rifampin: Effective against MRSA and intracellular S. aureus, with oral bioavailability suitable for outpatient treatment.
- Daptomycin + Ceftaroline or Cefepime: High cure rates in salvage therapy for recalcitrant cases.
- Clindamycin + Rifampin: Preferred in children and some MSSA infections with good tissue penetration and biofilm activity.
Evidence Supporting Antibiotic Synergy in Osteomyelitis
Several clinical and laboratory studies validate the use of synergistic antibiotic regimens in managing S. aureus osteomyelitis:
- In vitro time-kill studies have shown that combinations such as daptomycin + rifampin achieve bactericidal activity within 24 hours against biofilm-embedded MRSA.
- A retrospective cohort analysis (2022) indicated that patients receiving vancomycin-ceftaroline combinations had a 30% lower recurrence rate than vancomycin monotherapy.
- Randomized trials of rifampin-fluoroquinolone combinations for MSSA osteomyelitis show up to 90% cure rates in chronic cases.
Importance of Individualized Therapy and Synergy Testing
Empirical use of synergistic combinations should be guided by microbiological data, resistance patterns, and bone penetration profiles. The following diagnostic tools support synergy-based decision-making:
- Checkerboard assays: Quantify synergy via the fractional inhibitory concentration index (FICI).
- Time-kill curves: Evaluate bactericidal kinetics of drug pairs.
- E-test synergy strips: Rapid clinical tool to determine additive or synergistic effects.
Incorporating these methods enables the selection of combinations tailored to the pathogen and infection context.
Surgical Management and Antimicrobial Timing
Synergy alone is insufficient without surgical debridement or resection of necrotic tissue in chronic osteomyelitis. Antibiotic combinations should be initiated post-operatively, especially in the presence of prosthetic material or devascularized bone.
- Typical Duration: IV antibiotics for 6 weeks, followed by oral suppressive therapy where needed.
- Monitoring: Clinical signs, inflammatory markers (CRP, ESR), and imaging guide treatment response.
Challenges and Future Prospects in Synergy-Based Osteomyelitis Treatment
Despite advances, several barriers persist:
- Development of rifampin resistance with improper use
- Limited bone penetration of certain agents
- Toxicity from prolonged combination therapy
- Need for randomized controlled trials on newer synergistic regimens
Emerging solutions include:
- Localized antibiotic delivery (e.g., calcium sulfate beads with rifampin-daptomycin)
- Nanocarrier-enhanced delivery systems
- Bacteriophage-antibiotic synergy (PAS) under experimental evaluation
The treatment of staphylococcal osteomyelitis requires a comprehensive strategy that integrates surgical management with pharmacological precision. Synergistic antibiotic therapy—particularly those involving rifampin, glycopeptides, and lipopeptides—offers a substantial therapeutic advantage in penetrating biofilms, eliminating intracellular reservoirs, and preventing recurrence. Adopting personalized, evidence-backed synergistic regimens is vital in overcoming the complexities of this persistent and debilitating infection.