Pseudomonas aeruginosa is an opportunistic, Gram-negative, non-fermenting bacillus responsible for a subset of joint infections, particularly in immunocompromised individuals, intravenous drug users, or patients with prosthetic joints. The pathogen’s intrinsic resistance and its ability to form biofilms on joint tissues and prostheses make treatment particularly difficult. Synergistic antimicrobial therapy plays a critical role in overcoming resistance and enhancing eradication rates.
Pathogenesis and Risk Factors
Joint infections by P. aeruginosa can be classified as:
- Native joint septic arthritis, typically via hematogenous spread.
- Prosthetic joint infections (PJIs), often linked to surgical contamination or hematogenous seeding.
- Post-traumatic or post-surgical infections, especially after orthopedic hardware implantation.
Risk factors include:
- Diabetes mellitus
- Prolonged hospitalization or ICU stay
- Use of broad-spectrum antibiotics
- Immunosuppression
- Prior joint surgery or prosthesis
Challenges in Treating P. aeruginosa Joint Infections
This pathogen exhibits multiple resistance mechanisms:
- Efflux pumps that expel antibiotics
- Porin channel mutations reducing drug entry
- Biofilm formation, shielding the bacteria from immune cells and drugs
- Production of β-lactamases (including ESBLs and carbapenemases)
Consequently, monotherapy often fails, particularly in chronic or device-related infections. Combination antibiotic strategies are crucial for improving outcomes.
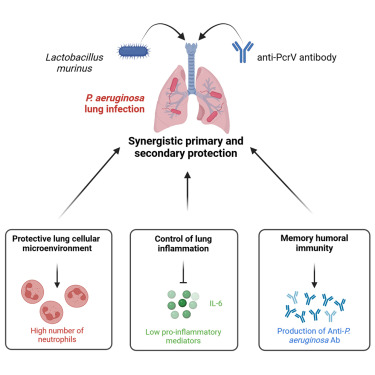
Rationale for Synergistic Antibiotic Therapy
Synergistic therapy involves using two or more antimicrobials whose combined effect exceeds the sum of their individual actions. This approach is essential in:
- Enhancing bacterial killing
- Preventing resistance development
- Disrupting mature biofilms
- Reaching avascular joint spaces and synovial fluid with adequate bactericidal concentrations
Effective Synergistic Combinations for Pseudomonas aeruginosa in Joint Infections
1. Beta-Lactam Plus Aminoglycoside
- Piperacillin-tazobactam + Amikacin/Gentamicin
- Broad coverage and proven synergy via disruption of cell wall (β-lactam) and inhibition of protein synthesis (aminoglycoside).
- Effective in initial empiric therapy for native and prosthetic joint infections.
2. Cefepime or Ceftazidime Plus Tobramycin
- Exhibits robust activity against P. aeruginosa and penetrates joint fluid effectively.
- Preferred in settings with moderate resistance but preserved susceptibility to cephalosporins.
3. Meropenem Plus Colistin
- Indicated in multidrug-resistant (MDR) or carbapenem-resistant P. aeruginosa strains.
- Colistin disrupts bacterial membranes; meropenem targets cell wall integrity.
4. Ceftolozane-tazobactam Plus Amikacin
- High efficacy against biofilm-producing and ESBL-producing strains.
- Clinical studies show strong synergism in persistent PJIs.
5. Aztreonam Plus Fosfomycin
- Considered in patients with β-lactam allergies.
- Fosfomycin enhances permeability, allowing aztreonam to bind effectively.
Clinical Evidence Supporting Synergy in Joint Infections
Numerous in vitro synergy studies and retrospective clinical analyses reinforce the value of combination therapy:
- A 2022 study in Infectious Diseases and Therapy demonstrated that ceftolozane-tazobactam with amikacin led to a 94% clinical cure rate in orthopedic infections involving P. aeruginosa.
- Checkerboard synergy testing shows that piperacillin-tazobactam with tobramycin consistently yields fractional inhibitory concentration index (FICI) < 0.5, indicating potent synergism.
- Time-kill studies confirm complete bacterial eradication within 24 hours with cefepime-amikacin in MDR isolates.
Surgical and Pharmacological Considerations
Surgical Management
- Debridement and irrigation are essential in septic arthritis.
- Exchange or removal of infected prosthesis in PJIs.
- Use of antibiotic-impregnated spacers during two-stage revisions.
Pharmacokinetic/Pharmacodynamic Considerations
- Ensure agents penetrate synovial fluid and avascular tissues.
- Monitor aminoglycoside levels to minimize toxicity.
- Adjust dosing in renal impairment, common in elderly or septic patients.
Duration and Monitoring of Therapy
- Native joint infections: 4–6 weeks of IV combination therapy.
- Prosthetic joint infections: Extended treatment up to 12 weeks, especially with retained hardware.
- Monitoring:
- Weekly CRP/ESR for inflammatory resolution
- Renal and hepatic panels
- Synovial fluid culture follow-up if clinical response is suboptimal
Future Directions in Managing Pseudomonas Joint Infections
Novel Therapeutics
- Cefiderocol: A siderophore cephalosporin with activity against MDR P. aeruginosa.
- Phage therapy: Emerging evidence in refractory prosthetic joint infections.
- Intra-articular antibiotic delivery: Localized, high-concentration therapy reducing systemic toxicity.
Personalized Synergy Testing
- Customized synergy testing panels tailored to isolate resistance patterns.
- Real-time diagnostic assays for rapid detection of β-lactamases and efflux pump overexpression.
Precision Synergy for Joint Infection Cure
Successful management of Pseudomonas aeruginosa joint infections hinges on timely initiation of synergistic antibiotic combinations, guided by susceptibility patterns and biofilm considerations. With growing antibiotic resistance, clinicians must adopt an aggressive yet targeted strategy combining pharmacological synergy, surgical intervention, and ongoing clinical monitoring. By integrating emerging therapies and personalized diagnostics, we can optimize treatment outcomes and preserve joint function in affected patients.