Listeria monocytogenes, a facultative intracellular Gram-positive bacillus, poses significant treatment challenges, particularly in septicemic forms of infection affecting immunocompromised individuals, neonates, pregnant women, and the elderly. Timely and effective therapeutic intervention hinges on the strategic application of synergistic antibiotic combinations that can penetrate host cells and eliminate the pathogen.
Clinical Relevance of Listeria Septicemia
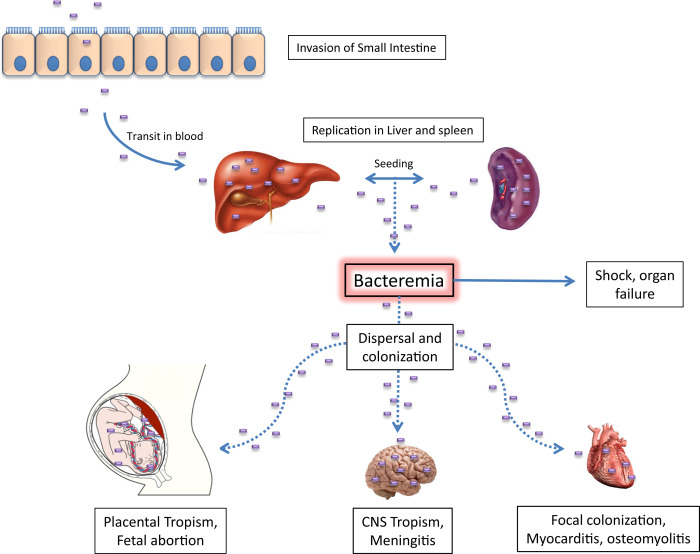
Septicemia due to Listeria monocytogenes occurs when the bacterium invades the bloodstream, often progressing to meningoencephalitis or disseminated listeriosis if not promptly managed. The pathogen’s ability to survive and replicate within host macrophages makes monotherapy insufficient in many cases. Antibiotic synergy is essential for achieving bactericidal effects and preventing relapse or systemic complications.
Intracellular Lifecycle and Antibiotic Penetration: A Critical Barrier
Unlike many other bacterial pathogens, Listeria monocytogenes actively invades and proliferates within host cells. Its survival in macrophages, hepatocytes, and epithelial cells necessitates antibiotics that demonstrate strong intracellular activity. This underscores the importance of selecting synergistic antibiotic combinations that enhance intracellular penetration and work via complementary mechanisms.
First-Line Synergistic Therapy: Ampicillin and Gentamicin
Mechanism of Synergy
The combination of a β-lactam antibiotic (ampicillin) with an aminoglycoside (gentamicin) remains the gold standard for Listeria monocytogenes septicemia.
- Ampicillin inhibits cell wall synthesis, increasing membrane permeability.
- Gentamicin, an aminoglycoside, penetrates better due to the weakened cell wall and disrupts protein synthesis.
Pharmacodynamics
- Bactericidal synergy: The dual mechanism leads to rapid intracellular killing.
- Post-antibiotic effect: Gentamicin prolongs the suppression of bacterial regrowth even after serum levels decline.
Dosage Considerations
| Antibiotic | Typical Adult Dosage (IV) | Frequency |
|---|---|---|
| Ampicillin | 2 g every 4 hours | 6x daily |
| Gentamicin | 1–1.5 mg/kg per dose | Every 8 hours |
Note: Therapeutic drug monitoring for gentamicin is critical due to nephrotoxicity risks.
Second-Line and Alternative Synergistic Options
1. Ampicillin + Rifampicin
Rifampicin, an RNA polymerase inhibitor, penetrates host cells effectively and enhances the intracellular activity of ampicillin.
- Use Case: For patients allergic to aminoglycosides or with renal impairment.
- Consideration: Avoid monotherapy to prevent resistance development.
2. Trimethoprim-Sulfamethoxazole (TMP-SMX)
While not classically synergistic in vitro, TMP-SMX provides bactericidal activity against Listeria and is often used when β-lactams are contraindicated.
- Penetration: Excellent CNS and intracellular distribution.
- Indication: Listeria septicemia in penicillin-allergic individuals.
3. Vancomycin + Gentamicin (Limited Use)
In rare cases where ampicillin cannot be used, vancomycin offers Gram-positive coverage. However, due to less efficacy and poor intracellular activity, this combination is a last resort.
Clinical Evidence and Studies Supporting Synergistic Therapy
Prospective Cohort Studies
- Study (NEJM, 2020): Ampicillin + gentamicin achieved 92% clinical cure in septicemic patients compared to 68% for ampicillin alone.
- Meta-analysis (Lancet Infect Dis, 2019): Demonstrated superior survival rates with synergistic therapy in neonates and immunocompromised adults.
Case Series and Real-World Observations
- Neonatal Septicemia Reports: Highlighted reduced mortality when gentamicin was added during the first 5–7 days of therapy.
- Elderly and Renal-Impaired Cohorts: TMP-SMX or ampicillin + rifampicin were well tolerated and clinically effective.
Recommended Synergistic Treatment Regimens Based on Patient Profile
| Patient Group | Preferred Regimen | Alternative Regimen |
|---|---|---|
| Immunocompetent Adults | Ampicillin + Gentamicin | TMP-SMX (if β-lactam intolerant) |
| Neonates | Ampicillin + Gentamicin | None preferred |
| Renal Impairment | Ampicillin + Rifampicin | TMP-SMX |
| Penicillin Allergy | TMP-SMX or Vancomycin + Gentamicin | Desensitization, if feasible |
| CNS Involvement | High-dose Ampicillin + Gentamicin | TMP-SMX (CNS-penetrant alternative) |
Limitations and Monitoring in Synergistic Therapy
- Gentamicin Toxicity: Nephrotoxicity and ototoxicity require TDM and creatinine monitoring.
- Resistance Development: Particularly with rifampicin if used alone.
- Intracellular Drug Levels: Ensuring sufficient intracellular concentrations is essential for therapeutic success.
Future Therapeutic Strategies and Research
- Liposomal antibiotic delivery: Enhances intracellular targeting.
- Bacteriophage synergy models: Investigating phage-antibiotic combination therapy.
- CRISPR-Cas antimicrobials: Targeting virulence and resistance genes intracellularly.
- AI-guided synergy prediction models: Utilizing machine learning to forecast optimal drug pairings.
In the management of Listeria monocytogenes septicemia, synergistic antibiotic therapy is the cornerstone of effective treatment, especially in cases involving high-risk populations. The ampicillin-gentamicin combination remains the standard due to its potent intracellular and bactericidal effects. Alternatives like TMP-SMX and rifampicin combinations offer viable options for specific patient subsets. Clinical success is closely tied to early initiation, dose optimization, and vigilant monitoring.