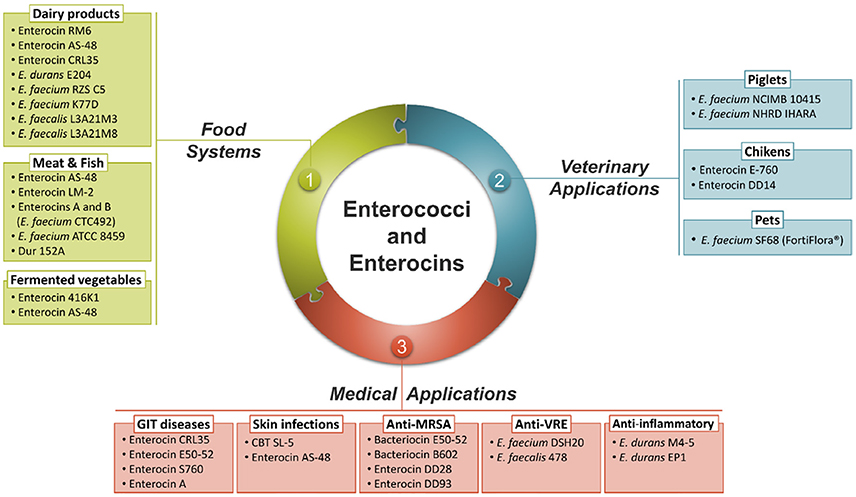
Enterococcal infections, primarily caused by Enterococcus faecalis and Enterococcus faecium, represent a significant challenge in clinical settings due to their inherent resistance mechanisms and capacity to acquire new resistances. These Gram-positive cocci are implicated in urinary tract infections, intra-abdominal infections, bacteremia, and infective endocarditis, with a high prevalence in nosocomial environments.
The use of synergistic antibiotic combinations is paramount to overcoming the limited bactericidal capacity of monotherapy and the emergence of multidrug-resistant (MDR) strains. Timely initiation of appropriate synergy-based regimens directly influences morbidity and mortality rates.
Antibiotic Synergy: The Foundation of Effective Enterococcal Therapy
The Importance of Synergistic Combinations
Unlike other Gram-positive bacteria, enterococci are intrinsically resistant to many antibiotics, including cephalosporins and low concentrations of aminoglycosides. Bactericidal activity is often achieved only through synergistic combinations, where two drugs exert greater effect together than individually.
Mechanistic Basis of Synergy
- Beta-lactams weaken the peptidoglycan layer, allowing aminoglycosides to penetrate the cell and inhibit protein synthesis.
- Dual beta-lactam therapy enhances PBP (penicillin-binding protein) saturation across multiple binding sites, resulting in bactericidal activity without reliance on nephrotoxic agents.
Key Synergistic Antibiotic Regimens for Enterococcal Infections
Ampicillin + Gentamicin
Use: Susceptible E. faecalis strains
Advantages: Proven bactericidal synergy
Limitations: Nephrotoxicity and ototoxicity risks; ineffective in HLAR strains
Monitoring: Trough and peak serum gentamicin levels essential
Ampicillin + Ceftriaxone
Use: HLAR E. faecalis or renal impairment
Advantages: Synergy without aminoglycoside toxicity
Mechanism: Dual PBP targeting
Clinical Evidence: Comparable efficacy to ampicillin-gentamicin in multiple studies
Vancomycin + Gentamicin
Use: Beta-lactam allergy or ampicillin-resistant Enterococcus faecium
Limitations: Higher toxicity; less preferred
Synergy: Suboptimal compared to ampicillin-based regimens
Daptomycin-Based Combinations
Use: MDR E. faecium, VRE (Vancomycin-resistant Enterococcus)
Suggested Combos:
- Daptomycin + Ampicillin
- Daptomycin + Ceftaroline
Rationale: Ampicillin enhances daptomycin binding through increased membrane permeability
Linezolid
Use: VRE when no synergistic beta-lactam combination is viable
Characteristics: Bacteriostatic, not synergistic; reserved for salvage therapy
Caution: Bone marrow suppression with prolonged use
Management of High-Level Aminoglycoside Resistance (HLAR)
HLAR is defined by a gentamicin MIC ≥500 μg/mL or streptomycin MIC ≥2000 μg/mL, rendering aminoglycosides ineffective, even in combination. This necessitates alternative regimens with demonstrated synergy.
Recommended Therapy for HLAR:
- Ampicillin + Ceftriaxone: First-line for HLAR E. faecalis
- Daptomycin-based therapy: For HLAR E. faecium with MDR profiles
- Avoid gentamicin or streptomycin-based regimens
Clinical Applications by Infection Site
1. Infective Endocarditis
- Native Valve, Susceptible: Ampicillin + Gentamicin for 4–6 weeks
- Prosthetic Valve or HLAR: Ampicillin + Ceftriaxone for 6 weeks
- MDR/VRE: Daptomycin (≥10 mg/kg) ± Ceftaroline or Linezolid
2. Bacteremia
- Empiric therapy should start with ampicillin-based combination
- De-escalate or modify based on susceptibility and HLAR status
- Duration: 2–4 weeks, depending on source and complications
3. Urinary Tract Infections
- Typically do not require synergistic therapy unless complicated or associated with bacteremia
- Consider high-dose ampicillin or nitrofurantoin based on susceptibility
Emerging Therapies and Resistance Surveillance
Newer agents and combination strategies are under investigation to combat MDR Enterococcus species, including:
- Tedizolid: Promising oxazolidinone with better tolerability than linezolid
- Eravacycline: Tetracycline derivative with activity against VRE
- β-lactam-enhanced daptomycin: A focus of ongoing clinical trials
Routine surveillance for resistance genes (e.g., vanA, aac(6′)-Ie-aph(2″)-Ia) is vital for guiding effective treatment decisions.
Toxicity Monitoring and Patient Safety
Close monitoring is essential for all synergistic regimens:
- Gentamicin: Nephrotoxicity, ototoxicity (monitor peaks/troughs, serum creatinine)
- Linezolid: Weekly CBCs for bone marrow suppression
- Daptomycin: Monitor CPK levels weekly to prevent rhabdomyolysis
- Ampicillin/Ceftriaxone: Generally well-tolerated, rare hypersensitivity
Surgical and Supportive Interventions
Adjunct surgical intervention may be necessary in:
- Refractory bacteremia or relapse
- Endocarditis with valve dysfunction
- Abscess formation or device-related infection
Supportive care should include hemodynamic stabilization, source control, and infection prevention strategies in hospital settings.
Effective treatment of enterococcal infections hinges on the strategic use of synergistic antibiotic combinations, especially in the presence of HLAR or MDR strains. Evidence supports the use of dual beta-lactam therapy and high-dose daptomycin combinations as potent alternatives to traditional aminoglycoside regimens. By implementing these optimized strategies with precision, we can significantly improve clinical outcomes and mitigate the burden of antibiotic resistance in enterococcal infections.