Enterobacter species, particularly Enterobacter cloacae and Enterobacter aerogenes, are opportunistic pathogens that can lead to meningitis, especially in individuals with compromised immune systems. Although Enterobacter meningitis is less common compared to other bacterial causes of meningitis, it poses significant clinical challenges due to its antibiotic resistance and the complexity of effective treatment options.
The purpose of this article is to provide an in-depth look at the synergistic approaches to treating Enterobacter meningitis, including the use of combination antibiotic therapy, adjunctive treatments, and supportive care strategies.
Pathogenesis and Risk Factors of Enterobacter Meningitis
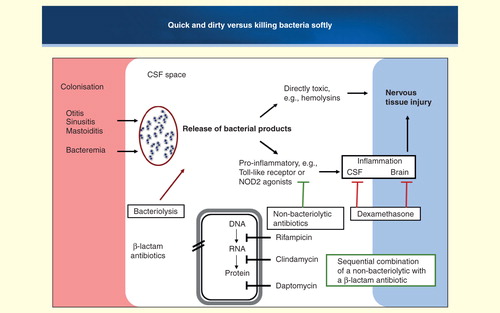
Enterobacter species typically cause meningitis through hematogenous spread or direct contamination, often following neurosurgical procedures or in patients with head trauma. The ability of Enterobacter species to produce beta-lactamases, enzymes that confer resistance to beta-lactam antibiotics, complicates the treatment regimen and often necessitates the use of combination antibiotic therapy to achieve a successful outcome.
Key Risk Factors for Enterobacter Meningitis
Several risk factors increase the likelihood of developing Enterobacter meningitis:
- Neurological surgery or head trauma, which provide direct access for the bacteria to enter the central nervous system.
- Premature infants and neonates, who are at higher risk due to their underdeveloped immune systems.
- Immunocompromised individuals, including those undergoing chemotherapy or organ transplantation.
- Underlying chronic conditions, such as diabetes mellitus and chronic kidney disease, which increase susceptibility to bacterial infections.
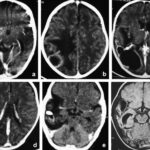
Diagnosis of Enterobacter Meningitis
An accurate and timely diagnosis is crucial to initiating the appropriate treatment for Enterobacter meningitis. The diagnostic approach generally involves a combination of clinical assessment, laboratory tests, and imaging studies.
Clinical Presentation
Patients with Enterobacter meningitis often exhibit the typical signs of bacterial meningitis, which include:
- Fever
- Severe headache
- Neck stiffness
- Photophobia
- Nausea and vomiting
- Altered mental status (confusion, irritability, or decreased responsiveness)
Laboratory Diagnosis
A lumbar puncture (LP) is the gold standard for diagnosing bacterial meningitis. The following findings are typically observed in cerebrospinal fluid (CSF) analysis:
- Increased white blood cell count (pleocytosis)
- Decreased glucose levels
- Elevated protein levels
- Positive culture or PCR results for Enterobacter species
In addition to CSF analysis, blood cultures and imaging studies (e.g., CT scans or MRI) may be performed to assess complications or identify other potential sources of infection.
Synergistic Antibiotic Therapy for Enterobacter Meningitis
Given the potential for antibiotic resistance in Enterobacter species, combination antibiotic therapy is often employed to enhance therapeutic efficacy. The synergistic effect of using multiple antibiotics can help overcome bacterial resistance mechanisms, such as the production of beta-lactamases, and ensure a more effective treatment approach.
Key Antibiotics in Enterobacter Meningitis Treatment
The following antibiotics are commonly used in the treatment of Enterobacter meningitis:
- Ceftriaxone and Cefotaxime: Third-generation cephalosporins are first-line options, effective against a wide range of Gram-negative organisms, including Enterobacter.
- Meropenem: A broad-spectrum carbapenem, meropenem is especially effective against extended-spectrum beta-lactamase (ESBL)-producing strains of Enterobacter.
- Vancomycin: Although primarily effective against Gram-positive bacteria, vancomycin may be included to address potential co-infections or resistant organisms.
- Gentamicin: This aminoglycoside is often combined with beta-lactam antibiotics to enhance bacterial killing, especially in severe infections like meningitis.
Synergistic Combinations for Enhanced Efficacy
Several antibiotic combinations have demonstrated synergistic effects in treating Enterobacter meningitis:
- Ceftriaxone + Gentamicin: This combination pairs ceftriaxone’s cell wall synthesis inhibition with gentamicin’s inhibition of protein synthesis, offering broad-spectrum coverage and enhancing bactericidal activity.
- Meropenem + Vancomycin: Meropenem, a carbapenem, targets bacterial cell wall synthesis, while vancomycin provides effective coverage against Gram-positive organisms, including potential Staphylococcus aureus co-infections.
- Cefotaxime + Trimethoprim-Sulfamethoxazole: This synergistic combination is effective against resistant strains of Enterobacter and is particularly beneficial in treating complicated infections.
The choice of antibiotic regimen depends on local resistance patterns, patient factors, and the susceptibility of the specific Enterobacter strain causing the infection.
Adjunctive Therapies in Enterobacter Meningitis Management
In addition to antibiotic therapy, adjunctive treatments are often used to manage inflammation, reduce intracranial pressure (ICP), and support overall patient recovery. These therapies are essential for improving clinical outcomes, especially in severe cases.
Corticosteroids for Inflammation Control
The use of corticosteroids, such as dexamethasone, is common in bacterial meningitis management to reduce inflammatory damage in the CNS. While studies suggest that corticosteroids are more beneficial for meningococcal and pneumococcal meningitis, their role in Enterobacter meningitis is still under investigation. However, corticosteroids may still be used in selected cases to prevent neurological complications.
Hyperosmolar Therapy: Mannitol and Hypertonic Saline
In cases where patients experience elevated intracranial pressure (ICP), mannitol or hypertonic saline can be used to reduce cerebral edema and improve brain perfusion. These agents are critical in preventing neurological deterioration and are frequently used in conjunction with antibiotic treatment.
Fluid and Electrolyte Management
Effective fluid management is essential to ensure adequate perfusion of vital organs and prevent dehydration during the treatment course. Monitoring renal function is especially important, as some antibiotics, such as aminoglycosides (e.g., gentamicin), can cause nephrotoxicity.
Prognosis and Long-Term Outcomes
The prognosis for patients with Enterobacter meningitis is influenced by several factors, including the timing of diagnosis, the effectiveness of antibiotic therapy, and the presence of underlying conditions. Early intervention and appropriate antibiotic treatment significantly improve patient outcomes, but delayed treatment can lead to severe complications.
Long-Term Neurological Complications
Despite prompt antibiotic therapy, some patients may experience long-term complications, including:
- Cognitive impairments: Difficulty with memory, concentration, and decision-making may persist in some patients.
- Seizures: Seizure activity can occur as a result of brain damage caused by the infection.
- Hearing loss: Permanent hearing loss is a well-documented complication of bacterial meningitis.
The use of corticosteroids and other supportive measures may help reduce the severity of these complications, although the results vary depending on the severity of the infection and the patient’s overall health.
The treatment of Enterobacter meningitis requires a multidimensional approach that includes synergistic antibiotic therapy, adjunctive treatments, and supportive care. The use of combination antibiotics is crucial for overcoming the bacterial resistance mechanisms often seen in Enterobacter species, ensuring effective treatment and improved clinical outcomes.
As antibiotic resistance continues to evolve, ongoing research into new therapeutic strategies and adjunctive therapies will be essential for optimizing the management of Enterobacter meningitis. By providing a comprehensive treatment plan, healthcare professionals can significantly improve the prognosis for patients affected by this serious and challenging infection.