Castration-resistant prostate cancer (CRPC) is a form of prostate cancer that continues to progress despite androgen deprivation therapy (ADT), which is a cornerstone treatment for advanced prostate cancer. Understanding the complexities of CRPC, its treatment options, and management strategies is vital for healthcare professionals and patients alike.
What is Castration-Resistant Prostate Cancer?
CRPC is defined by disease progression despite the suppression of androgens, hormones that fuel prostate cancer growth. It can present as a rising prostate-specific antigen (PSA) level, radiographic progression, or symptomatic advancement, even with testosterone levels reduced to castrate levels (≤20 ng/dL).
Key Characteristics of CRPC
- Hormone Independence: Tumor growth occurs even with suppressed androgen levels.
- Variable Progression: CRPC may be localized or metastatic (mCRPC).
- PSA Dynamics: Rising PSA levels often signal disease progression, but PSA changes do not always correlate with clinical outcomes.
Risk Factors and Diagnosis
Risk Factors
- Advanced Prostate Cancer: A history of prostate cancer with initial hormone sensitivity.
- Incomplete Androgen Suppression: Persistent low levels of circulating androgens.
- Genetic Mutations: Variants in genes like BRCA1, BRCA2, or ATM may increase risk.
Diagnostic Criteria
CRPC diagnosis involves a combination of laboratory and imaging studies:
- PSA Progression: A confirmed rise in PSA on three consecutive measurements taken at least one week apart.
- Radiographic Evidence: New lesions on bone scans or soft tissue progression on CT/MRI.
- Symptomatology: Worsening symptoms despite optimal ADT.
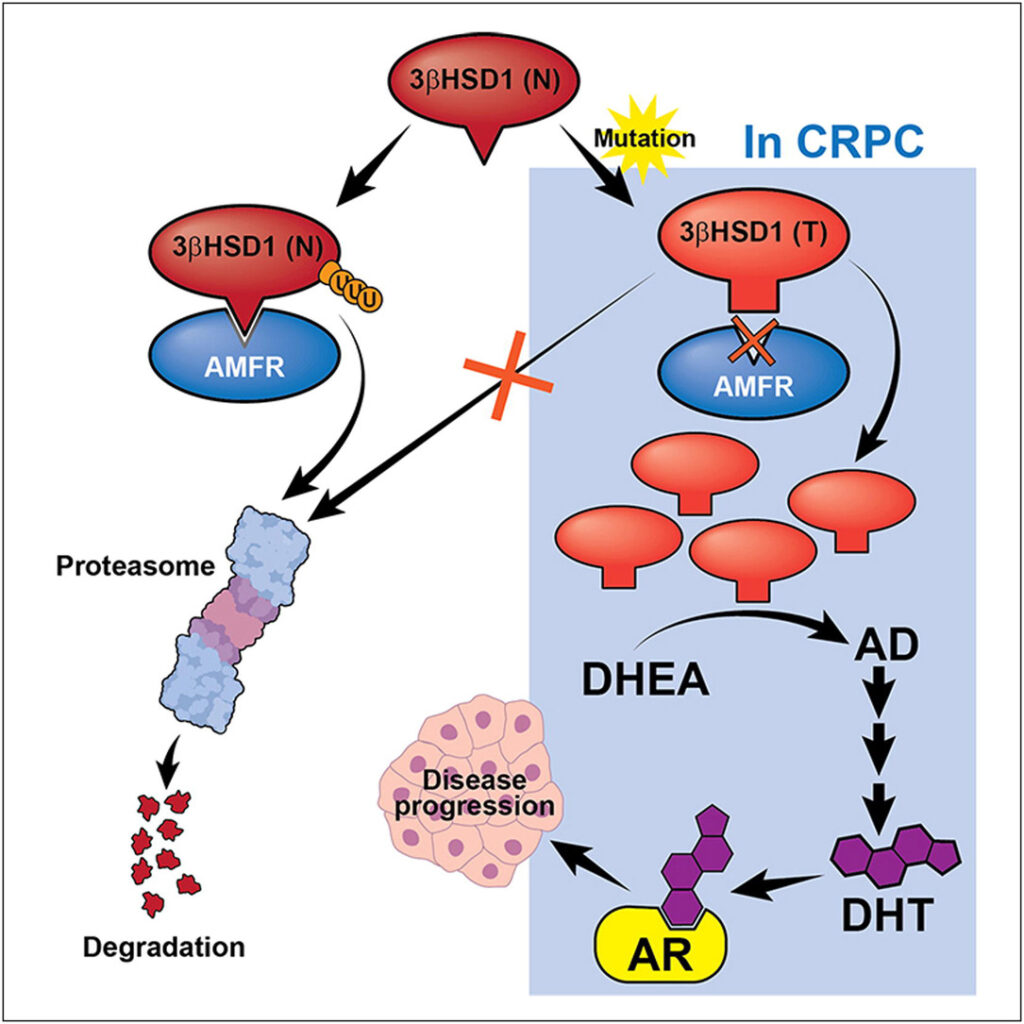
Pathophysiology of CRPC
The progression to CRPC involves several mechanisms:
- Androgen Receptor (AR) Pathway Activation: AR amplification and mutations enable cancer cells to utilize minimal androgen levels.
- Intratumoral Androgen Synthesis: Tumor cells produce their own androgens.
- Alternative Growth Pathways: Activation of pathways like PI3K/AKT/mTOR bypasses AR dependence.
graph LR
A[Androgen Deprivation Therapy] --> B[Reduced Testosterone Levels]
B --> C[AR Mutations]
B --> D[Intratumoral Androgen Synthesis]
C --> E[Continued Tumor Growth]
D --> ETreatment Strategies for CRPC
Systemic Therapies
- Androgen Receptor-Targeted Agents
- Enzalutamide: Inhibits AR signaling by blocking androgen binding.
- Abiraterone Acetate: Suppresses androgen biosynthesis.
- Chemotherapy
- Docetaxel: A first-line chemotherapeutic agent for mCRPC.
- Cabazitaxel: Used after docetaxel resistance.
- Bone-Targeted Therapies
- Radium-223 Dichloride: Treats bone metastases and improves survival.
- Bisphosphonates and Denosumab: Prevent skeletal-related events.
- Immunotherapy
- Sipuleucel-T: An autologous cellular immunotherapy.
- PARP Inhibitors
- Effective in patients with BRCA1/2 or ATM mutations.
Emerging Therapies
- Targeted Radioligand Therapy: PSMA-targeted agents like lutetium-177.
- Combination Therapies: Investigating synergistic effects of AR inhibitors and immune checkpoint inhibitors.
Monitoring and Prognosis
Monitoring Response to Treatment
- PSA Levels: Regular monitoring to assess biochemical response.
- Imaging Studies: Periodic CT, MRI, and bone scans.
- Clinical Symptoms: Evaluation of pain, fatigue, and quality of life.
Prognostic Indicators
- Baseline PSA Levels: Higher levels often indicate poorer outcomes.
- Extent of Metastases: Bone and visceral metastases have varying prognostic implications.
- Molecular Markers: Mutational analysis for personalized treatment approaches.
Managing Quality of Life in CRPC Patients
Addressing Symptoms
- Pain Management: Use of opioids, non-opioid analgesics, and bone-targeted therapies.
- Fatigue Mitigation: Exercise programs and psychological support.
Supportive Care
- Nutritional Counseling: Maintaining a healthy diet to manage treatment side effects.
- Psychosocial Support: Access to counseling and support groups.