Strongyloidiasis is a parasitic infection caused by the nematode Strongyloides stercoralis, a roundworm that primarily affects the human gastrointestinal system. This infection is a major concern in tropical and subtropical regions, although it can occur worldwide, particularly in individuals who live in or travel to endemic areas. The parasite can lead to a range of symptoms, some of which may be severe and even fatal, particularly in immunocompromised individuals.
Understanding strongyloidiasis involves recognizing its transmission, the lifecycle of the parasite, common symptoms, diagnosis, treatment options, and methods of prevention. This guide offers in-depth insights into each of these aspects to help mitigate the risks associated with this infection.
The Lifecycle and Transmission of Strongyloides stercoralis
Strongyloidiasis is a unique parasitic infection due to the ability of Strongyloides stercoralis to complete its lifecycle both inside and outside the human body. The lifecycle begins when the larvae present in contaminated soil or feces come into contact with the skin of a host. This typically occurs when a person walks barefoot in contaminated environments.
Lifecycle Stages of Strongyloides stercoralis:
- Larval Stage: The larvae penetrate the skin and enter the bloodstream, traveling to the lungs. From there, they migrate to the throat, where they are swallowed.
- Adult Worm Stage: Once in the intestines, the larvae mature into adult female worms, which produce eggs that hatch into larvae. These larvae either exit the body through the stool or can reinfect the host by penetrating the intestinal lining, leading to autoinfection.
- Autoinfection: This is a unique aspect of S. stercoralis, where larvae in the intestines can re-enter the bloodstream and begin the cycle again, potentially leading to chronic infection.
The continuous cycle of reinfection can result in the persistence of strongyloidiasis in a host, particularly when the immune system is not functioning optimally.
Symptoms of Strongyloidiasis
The symptoms of strongyloidiasis can vary widely, from mild to severe, depending on the stage of the infection and the health of the individual. Some people may remain asymptomatic for long periods, while others experience significant illness.
Common Symptoms of Acute Strongyloidiasis:
- Abdominal pain: A common symptom due to the presence of larvae in the gastrointestinal tract.
- Diarrhea: Often watery, it can occur alongside other gastrointestinal symptoms.
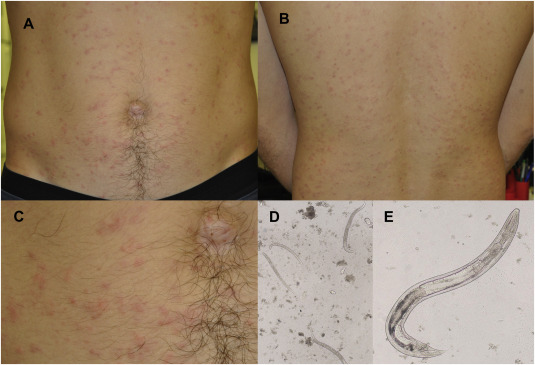
- Skin rashes: Itchy, raised red areas known as “larva currens” are indicative of larvae migrating under the skin.
- Cough and wheezing: This can occur when larvae migrate through the lungs during their lifecycle.
Chronic Strongyloidiasis Symptoms:
In chronic cases, S. stercoralis can lead to a condition known as hyperinfection syndrome, particularly in immunocompromised individuals such as those with HIV/AIDS, organ transplant recipients, or those on immunosuppressive therapies. Symptoms can include:
- Severe gastrointestinal symptoms: Including persistent abdominal pain, bloating, and diarrhea.
- Respiratory distress: Due to the overwhelming migration of larvae through the lungs.
- Sepsis: A life-threatening infection in the bloodstream that can result from bacterial translocation due to compromised intestinal integrity.
Diagnosis of Strongyloidiasis
Strongyloidiasis is often challenging to diagnose, particularly in the absence of clear symptoms. A thorough medical history, especially regarding travel to endemic areas, is essential. Diagnostic techniques typically include:
Laboratory Tests for Diagnosis:
- Stool Examination: Microscopic examination of stool samples for larvae is a common diagnostic method. Multiple stool samples may be required to detect the larvae, as they are not consistently shed.
- Serological Tests: Blood tests that detect antibodies to Strongyloides stercoralis can help identify infection, even in cases with no obvious symptoms.
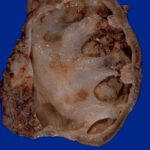
- Duodenal Aspiration or Biopsy: In cases where stool examination is inconclusive, aspirating fluid from the duodenum or performing a biopsy may reveal larvae.
- PCR Testing: Polymerase chain reaction (PCR) can detect S. stercoralis DNA, providing a highly sensitive diagnostic method.
Treatment Options for Strongyloidiasis
Treatment for strongyloidiasis is crucial, particularly in preventing complications such as hyperinfection syndrome. The primary medication used to treat this infection is ivermectin, which is highly effective in eliminating the larvae and preventing further spread.
Medications Used for Strongyloidiasis:
- Ivermectin: The drug of choice for treating Strongyloides stercoralis infection. It is typically administered in a single dose, though additional doses may be required in some cases.
- Albendazole: An alternative to ivermectin, this medication may be used if the patient cannot tolerate ivermectin.
- Thiabendazole: Another option for treatment, though less commonly used due to its side effects.
Treatment for Hyperinfection Syndrome:
In patients with hyperinfection syndrome or disseminated strongyloidiasis, more aggressive treatment may be required. This often involves a longer course of ivermectin or a combination of ivermectin and albendazole, along with supportive care.
Prevention of Strongyloidiasis
Preventing strongyloidiasis primarily involves avoiding exposure to environments where S. stercoralis larvae are prevalent. Key preventive measures include:
Key Prevention Strategies:
- Avoid walking barefoot: In areas where soil contamination is common, wearing shoes can prevent skin contact with larvae.
- Improved sanitation: Ensuring proper sanitation and waste disposal in endemic regions can help reduce soil contamination.
- Hygiene practices: Washing hands regularly and maintaining proper hygiene can reduce the risk of ingestion of contaminated food or water.
- Screening and treating at-risk populations: People who are immunocompromised or who have traveled to endemic areas should be screened for Strongyloides and treated if necessary.
The Impact of Strongyloidiasis on Global Health
Strongyloidiasis is often underreported and overlooked in global health discussions, but it poses a significant burden in tropical and subtropical regions. The infection affects millions of people worldwide, with particular concern for those in developing nations with poor sanitation and healthcare infrastructure.
While the condition is treatable, the high rate of chronic infections, particularly in immunocompromised individuals, requires increased awareness and investment in global health initiatives aimed at improving sanitation, access to healthcare, and early diagnosis and treatment.
Strongyloidiasis, caused by Strongyloides stercoralis, remains a significant parasitic infection that requires prompt diagnosis and treatment to prevent serious complications, especially in immunocompromised individuals. By understanding the lifecycle, symptoms, diagnosis, treatment options, and prevention methods for strongyloidiasis, healthcare professionals can better manage and reduce the impact of this parasitic disease. Continued research, public health efforts, and education are essential to minimizing the spread and improving the outcomes for individuals affected by strongyloidiasis.