Carnitine deficiency is a metabolic condition that occurs when the body lacks sufficient carnitine, a compound essential for energy production. This article explores its causes, symptoms, diagnosis, and treatment options, providing a thorough understanding for individuals seeking clarity and solutions.
Carnitine is a naturally occurring compound synthesized in the liver and kidneys from amino acids lysine and methionine. It plays a vital role in transporting long-chain fatty acids into the mitochondria, where they are oxidized to produce energy. Additionally, carnitine helps remove toxic compounds from cells, preventing their accumulation.
Types
Can be categorized into two primary types:
Primary Carnitine Deficiency
This is a rare genetic disorder caused by mutations in the SLC22A5 gene, which encodes the carnitine transporter protein. Individuals with this condition are unable to effectively transport carnitine into cells, leading to low carnitine levels despite normal dietary intake.
Secondary Carnitine Deficiency
Secondary deficiency occurs due to external factors that reduce carnitine levels. Common causes include:
- Chronic illnesses (e.g., kidney or liver disease)
- Certain medications (e.g., valproic acid, antibiotics)
- Nutritional deficiencies
- Metabolic disorders
- Premature birth
Symptoms
The clinical presentation of carnitine deficiency varies depending on its severity and type. Common symptoms include:
- Muscle weakness and fatigue
- Hypoglycemia
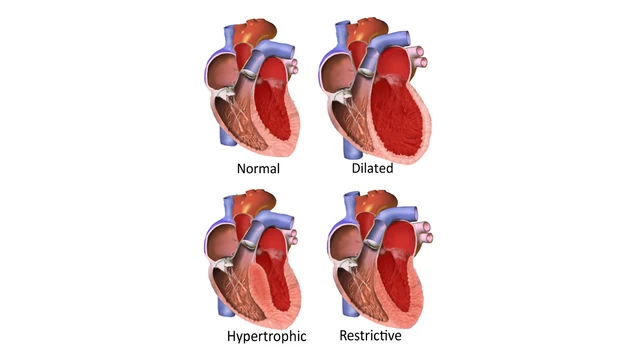
- Cardiomyopathy
- Developmental delays (in children)
- Recurrent infections
- Hepatomegaly (enlarged liver)
Early diagnosis is crucial to prevent severe complications, such as organ failure and metabolic crises.
Diagnosing
Medical History and Physical Examination
Physicians assess a patient’s medical history, including family history of metabolic disorders, and perform a thorough physical examination.
Laboratory Tests
Key diagnostic tests include:
- Plasma Free Carnitine Levels: Measures carnitine concentration in blood.
- Acylcarnitine Profile: Identifies specific metabolic abnormalities.
- Genetic Testing: Detects mutations in the SLC22A5 gene.
Additional Assessments
Other diagnostic tools, such as echocardiograms and liver function tests, may be used to evaluate organ involvement.
Treatment Options
Treatment for carnitine deficiency focuses on replenishing carnitine levels and managing symptoms.
Carnitine Supplementation
Oral or intravenous L-carnitine supplements are the cornerstone of treatment. Dosage varies based on the severity of the deficiency and patient age.
Dietary Modifications
A well-balanced diet rich in carnitine-containing foods, such as red meat, fish, poultry, and dairy products, can support carnitine levels. For individuals with secondary deficiency, addressing underlying conditions is essential.
Management of Underlying Causes
Treating conditions like kidney or liver disease and adjusting medication regimens can help restore normal carnitine levels.
Monitoring and Long-term Care
Regular follow-ups with healthcare providers ensure optimal management and early detection of complications.
Specific Populations
Infants and Children
In newborns and young children, carnitine deficiency may manifest as developmental delays, failure to thrive, and recurrent infections. Early screening is critical for prompt intervention.
Pregnant Women
Pregnancy can exacerbate carnitine deficiency due to increased metabolic demands. Supplementation and monitoring are recommended for affected individuals.
Athletes
Although rare, athletes may experience secondary carnitine deficiency due to intense physical activity and inadequate dietary intake.
Prevention
Preventive measures include:
- Consuming a diet rich in carnitine
- Regular health check-ups
- Genetic counseling for at-risk families
- Avoiding medications that deplete carnitine, when possible

