Streptococcus osteomyelitis refers to a serious bacterial bone infection caused predominantly by species of Streptococcus, particularly Streptococcus pyogenes (Group A Streptococcus, GAS), Streptococcus agalactiae (Group B Streptococcus, GBS), and occasionally Streptococcus pneumoniae. While Staphylococcus aureus remains the most common causative organism of osteomyelitis, streptococcal species are increasingly recognized in both pediatric and adult populations, often presenting with an acute course and significant systemic involvement.
Pathogenesis of Streptococcal Bone Infections
Streptococcus species invade bone through one of three main routes: hematogenous spread, direct inoculation (trauma or surgery), or contiguous spread from adjacent soft tissue infections. Once within the bone matrix, bacterial proliferation incites an intense inflammatory response, leading to bone necrosis, periosteal elevation, and possible formation of sequestra.
Key Virulence Factors
- M protein (GAS): Inhibits phagocytosis and promotes immune evasion
- Capsular polysaccharides (GBS): Prevent opsonization
- Exotoxins and enzymes: Facilitate tissue invasion and degradation
- Biofilm formation: Enhances persistence in chronic osteomyelitis
Epidemiology of Streptococcus Osteomyelitis
- Children: Hematogenous osteomyelitis is more common, with long bones (femur, tibia) being the primary sites.
- Adults: More frequently associated with trauma, surgery, or contiguous infections.
- Immunocompromised hosts: At higher risk for GBS and polymicrobial infections.
Clinical Presentation and Symptoms
Acute Osteomyelitis:
- Sudden onset of bone pain, localized swelling, and warmth
- Fever, malaise, and irritability (especially in children)
- Limited range of motion in adjacent joints
- Elevated inflammatory markers (CRP, ESR, leukocytosis)
Chronic Osteomyelitis:
- Persistent or intermittent bone pain
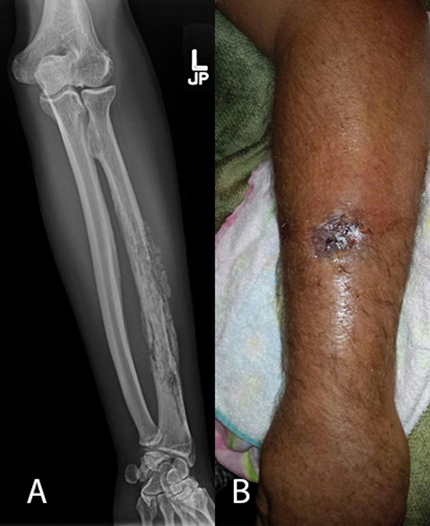
- Draining sinus tracts or non-healing ulcers
- Radiographic evidence of cortical destruction and sequestrum
- May occur after incomplete treatment of acute infection
Common Sites of Infection
| Population | Common Bones Affected |
|---|---|
| Pediatric | Femur, tibia, humerus |
| Adults | Vertebrae, pelvis, foot |
| Diabetics | Tarsal and metatarsal bones |
| IV drug users | Spine, clavicle |
Diagnostic Approach to Streptococcus Osteomyelitis
Laboratory Studies:
- CBC: Leukocytosis with neutrophilia
- CRP and ESR: Elevated in acute and chronic infections
- Blood cultures: Often positive in hematogenous cases
- Bone biopsy: Gold standard for microbial identification and antibiotic sensitivity
Imaging Modalities:
- Plain X-ray: May show lytic lesions after 10–14 days
- MRI: Most sensitive for early detection; shows marrow edema and abscess formation
- CT scan: Useful for surgical planning and detecting sequestra
- Radionuclide bone scans: Helpful when MRI is contraindicated
Microbiological Identification
- Aerobic cultures: From bone biopsy or aspirated pus
- Anaerobic cultures: Important in polymicrobial cases
- PCR-based assays: May identify fastidious or slow-growing streptococci
- Serologic tests: Rarely used but may support GAS diagnosis (e.g., anti-streptolysin O titers)
Treatment and Antibiotic Management
Empirical Antibiotic Therapy
Should be initiated after obtaining cultures but not delayed if the patient is septic:
- Penicillin G or Ceftriaxone (for GAS and GBS)
- Add Clindamycin if toxin suppression is needed
- Vancomycin added if MRSA or resistant streptococci are suspected
Tailored Therapy (Post-Culture Results):
- Duration: 4–6 weeks of IV antibiotics; may transition to oral agents based on clinical response
- Chronic Osteomyelitis: Often requires longer courses, especially if surgical debridement is incomplete
Surgical Intervention
Surgery is often required in cases of:
- Abscess formation
- Necrotic bone requiring removal (sequestrectomy)
- Chronic infection with draining sinuses
- Failure of medical therapy
Surgical procedures include:
- Debridement: Removal of infected and necrotic tissue
- Bone grafting: Reconstruction after excision
- Stabilization: In cases of bone instability or pathologic fracture
Prognosis and Outcomes
With timely diagnosis and appropriate management, the prognosis for acute streptococcal osteomyelitis is generally favorable. However, delayed treatment may lead to:
- Chronic osteomyelitis
- Growth disturbances in children
- Functional impairment
- Amputation in severe or uncontrolled cases
Risk factors for poor outcomes include diabetes mellitus, peripheral vascular disease, immunosuppression, and prior incomplete therapy.
Prevention Strategies
- Prompt treatment of soft tissue and skin infections
- Careful wound hygiene after trauma or surgery
- Antibiotic prophylaxis in high-risk surgical procedures
- Monitoring and early intervention in patients with systemic streptococcal infections
Streptococcus osteomyelitis represents a serious but manageable infection of the bone, requiring high clinical suspicion, especially in cases of unexplained bone pain with systemic symptoms. Early diagnosis, precise identification of the pathogen, and aggressive antibiotic therapy—often supplemented by surgical debridement—are crucial for optimal recovery. Understanding the pathogenic mechanisms and risk factors aids in early recognition and prevention, reducing the burden of this potentially debilitating disease.