A Streptococcus lung abscess is a localized collection of pus within the lung parenchyma caused by Streptococcus species. It typically arises due to necrotizing pneumonia and is characterized by cavitary lesions, often with air-fluid levels, visible on imaging. This condition is particularly concerning due to its potential for rapid progression, especially in immunocompromised patients or individuals with poor dental hygiene, aspiration risk, or chronic pulmonary diseases.
Etiological Agents: Streptococcal Species in Lung Abscess Formation
Streptococcus pneumoniae
Though an uncommon cause of cavitary disease, virulent strains, especially serotype 3 and 19A, can lead to necrotizing pneumonia with abscess formation.
Streptococcus anginosus group (SAG)
Members such as S. anginosus, S. intermedius, and S. constellatus are microaerophilic and known for their abscess-forming tendency. They are frequently involved in polymicrobial infections, especially following aspiration.
Streptococcus pyogenes (Group A Streptococcus)
Capable of producing severe, rapidly progressing necrotic infections due to cytotoxins such as streptolysin O and exotoxins, though rare in pulmonary abscesses.
Pathophysiology of Streptococcus Lung Abscess
Lung abscesses result from localized suppurative necrosis of pulmonary tissue. Infections typically begin as aspiration pneumonia, particularly in the posterior upper lobes or superior lower lobes, and progress to abscess due to:
- Enzymatic tissue destruction by bacterial virulence factors
- Impaired host immune response
- Delayed treatment or antibiotic resistance
Clinical Manifestations of Streptococcus Lung Abscess
Common Symptoms:
- Persistent, productive cough with foul-smelling or purulent sputum
- High-grade fever and chills
- Night sweats and weight loss
- Pleuritic chest pain
- Hemoptysis in some cases
Physical Findings:
- Decreased breath sounds
- Rales or crackles over affected area
- Signs of consolidation or cavitation
Symptoms typically evolve over weeks unless the infection is aggressively progressive, as with certain S. pyogenes strains.
Diagnostic Evaluation of Streptococcus Lung Abscess
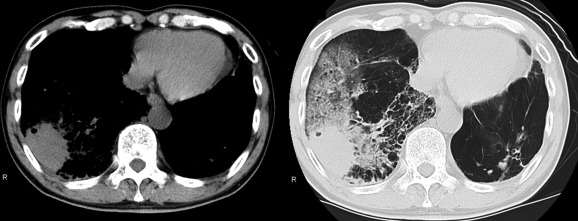
Imaging Studies:
- Chest X-Ray: Shows a cavitary lesion with an air-fluid level
- CT Chest with Contrast: Gold standard for defining abscess location, wall thickness, and differentiating from empyema or malignancy
Microbiological Tests:
- Sputum Culture and Gram Stain: May reveal gram-positive cocci in chains; anaerobes often coexist
- Blood Cultures: Especially in systemic illness
- Bronchoscopy with BAL (Bronchoalveolar Lavage): Helpful for deeper sampling and culture
- Pleural Fluid Analysis (if associated effusion present)
PCR and advanced molecular techniques improve detection, particularly for non-culturable or fastidious streptococcal species.
Treatment Protocols for Streptococcus Lung Abscess
Empirical Antibiotic Therapy:
Initial broad-spectrum coverage should address both aerobes and anaerobes, especially in aspiration-related cases:
- Beta-lactam/beta-lactamase inhibitors: e.g., Ampicillin-sulbactam
- Carbapenems: e.g., Imipenem, especially in hospital-acquired or resistant strains
- Clindamycin: Excellent anaerobic and some gram-positive coverage
- Vancomycin: For suspected MRSA or drug-resistant S. pneumoniae
Targeted Therapy:
Based on culture and sensitivity results:
- S. pneumoniae: High-dose penicillin G, ceftriaxone, or levofloxacin
- SAG: Sensitive to penicillin, amoxicillin-clavulanate
- S. pyogenes: Penicillin + clindamycin
Duration: Typically 4–6 weeks, depending on radiological resolution and clinical improvement.
Interventional and Surgical Management
Most streptococcal lung abscesses resolve with medical management; however, intervention is required in selected cases.
Indications for Intervention:
- No clinical/radiological improvement in 7–10 days
- Large abscess (>6 cm)
- Hemorrhagic complications or rupture into pleural space
- Suspicion of neoplasm or unresolved infection
Procedures:
- Percutaneous catheter drainage: Under CT or ultrasound guidance
- Bronchoscopy: For airway clearance or obstruction management
- Lobectomy or segmentectomy: Reserved for refractory or complicated cases
Complications of Untreated or Severe Lung Abscess
- Empyema thoracis
- Bronchopleural fistula
- Chronic lung abscess
- Sepsis and multi-organ dysfunction
- Cavitation leading to massive hemoptysis
- Pulmonary fibrosis or structural damage
Prompt recognition and aggressive treatment significantly reduce the risk of these sequelae.
Preventive Strategies and Risk Factor Modification
Prevent Aspiration:
- Elevate head of bed in at-risk patients
- Manage swallowing dysfunction
- Control alcohol and substance abuse
Dental and Respiratory Hygiene:
- Regular dental care reduces oropharyngeal bacterial load
- Treat underlying conditions like COPD, bronchiectasis, or cystic fibrosis
Immunization:
- Pneumococcal vaccine reduces incidence of invasive pneumococcal disease and complications like lung abscess
Prognosis of Streptococcus Lung Abscess
With appropriate and timely treatment, the prognosis is generally favorable. The majority of patients experience complete resolution without the need for surgery. Factors associated with poorer outcomes include:
- Advanced age
- Comorbidities (e.g., diabetes, malignancy)
- Delayed initiation of antibiotics
- Infection with toxin-producing strains
- Incomplete source control
Streptococcus lung abscess is a serious pulmonary infection requiring a high index of suspicion, particularly in patients with aspiration risk or unresolved pneumonia. S. pneumoniae, SAG, and S. pyogenes are the principal pathogens, capable of causing extensive tissue necrosis. Management requires a combination of prolonged antibiotic therapy, radiological monitoring, and, in some cases, interventional drainage. Early intervention and tailored therapy remain the cornerstone of effective clinical outcomes.