Atrial flutter is a common cardiac arrhythmia characterized by a rapid and irregular atrial rhythm. Left untreated, it may lead to complications such as stroke, heart failure, or chronic atrial fibrillation. Cardioversion is a primary treatment strategy aimed at restoring normal sinus rhythm. This article explores the intricacies of cardioversion for atrial flutter, including indications, methods, risks, and post-procedure care.
Understanding Atrial Flutter
What is Atrial Flutter?
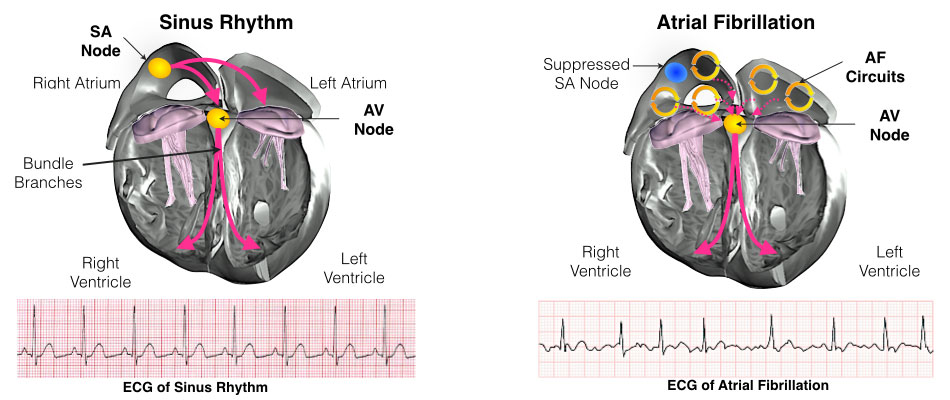
Atrial flutter occurs due to a reentrant circuit in the atria, causing the heart to beat at an abnormally fast rate. This condition compromises cardiac efficiency and can result in symptoms such as palpitations, fatigue, shortness of breath, and dizziness.
Causes and Risk Factors
- Structural Heart Diseases: Conditions like coronary artery disease and valvular disorders.
- Lifestyle Factors: Excessive alcohol consumption and smoking.
- Underlying Conditions: Hyperthyroidism, obesity, and sleep apnea.
Diagnosis
Atrial flutter is typically diagnosed using:
- Electrocardiography (ECG): Demonstrates characteristic “sawtooth” flutter waves.
- Echocardiography: Evaluates structural abnormalities.
- Holter Monitoring: Detects intermittent episodes.
Cardioversion: An Overview
What is Cardioversion?
Cardioversion is a procedure used to convert an irregular heart rhythm back to normal sinus rhythm. For atrial flutter, cardioversion may be performed either electrically or pharmacologically.
Methods of Cardioversion
Electrical Cardioversion
Electrical cardioversion involves the delivery of synchronized electrical shocks to the heart to reset its rhythm.
Procedure
- Preparation: Patients are sedated, and anticoagulation therapy is initiated if necessary.
- Electrode Placement: Paddles or patches are positioned on the chest.
- Shock Delivery: A synchronized shock is delivered at the appropriate phase of the cardiac cycle to avoid ventricular fibrillation.
Indications
- Persistent atrial flutter causing hemodynamic instability.
- Failure of pharmacological cardioversion.
Benefits
- High efficacy with success rates exceeding 90%.
- Immediate restoration of rhythm.
Pharmacological Cardioversion
This method uses antiarrhythmic drugs to achieve rhythm control.
Common Medications
- Ibutilide: Highly effective in atrial flutter but requires close monitoring for QT prolongation.
- Amiodarone: A versatile agent used for rhythm conversion and maintenance.
Limitations
- Lower efficacy compared to electrical cardioversion.
- Potential for drug-related adverse effects.
Risks and Complications
While generally safe, cardioversion carries some risks:
Short-Term Risks
- Thromboembolic Events: Risk of stroke, mitigated by adequate anticoagulation.
- Arrhythmias: Rarely, new or worsening arrhythmias may occur.
Long-Term Risks
- Recurrence: Atrial flutter may recur, necessitating further intervention.
- Cardiac Damage: Uncommon but possible with repeated procedures.
Anticoagulation and Cardioversion
Effective anticoagulation is crucial to minimize thromboembolic risk.
Pre-Procedure
- Patients with atrial flutter for >48 hours require anticoagulation for at least 3 weeks prior.
Post-Procedure
- Continuation of anticoagulation for 4 weeks post-cardioversion is recommended.
Recovery and Follow-Up
Post-procedure care is vital to ensure long-term success and patient safety.
Immediate Recovery
- Monitoring in a cardiac care unit for a few hours post-procedure.
- Managing potential side effects such as transient fatigue or mild chest discomfort.
Long-Term Management
- Addressing underlying causes to prevent recurrence.
- Regular follow-ups with a cardiologist to monitor rhythm and anticoagulation status.