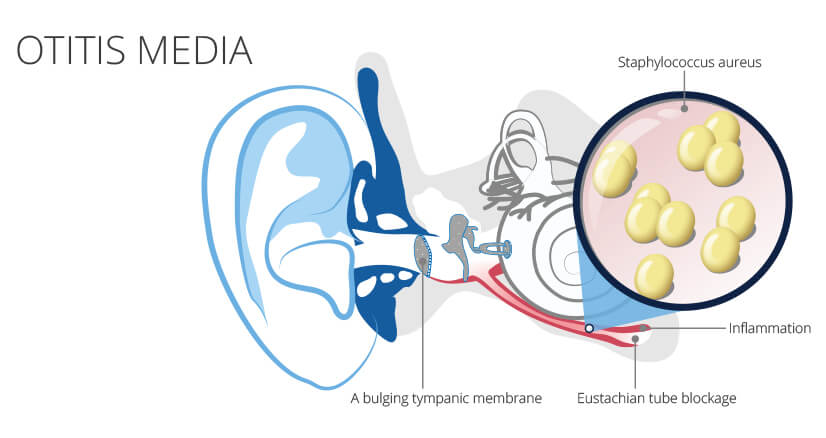
Staphylococcus acute otitis media (AOM) refers to an infection of the middle ear caused by Staphylococcus aureus, including methicillin-resistant strains (MRSA). Although less common than pneumococcal or Haemophilus influenzae-related AOM, staphylococcal etiologies demand heightened clinical attention due to their aggressive nature, resistance patterns, and potential for complications. Timely recognition and targeted therapy are essential in managing this condition effectively.
Overview of Staphylococcal Acute Otitis Media
Definition and Epidemiology
Acute otitis media is an inflammatory condition of the middle ear, typically presenting with rapid onset of signs and symptoms such as ear pain, fever, and tympanic membrane abnormalities. While S. pneumoniae and H. influenzae are more prevalent causes, Staphylococcus aureus — particularly MRSA — has become increasingly implicated, especially in recurrent or treatment-resistant cases.
Risk Populations
- Infants and children under 3 years of age
- Individuals with frequent upper respiratory infections
- Patients with tympanostomy tubes or recent otologic surgery
- Immunocompromised hosts
- Hospitalized or institutionalized individuals
Pathophysiology of Staphylococcal Ear Infections
The pathogenesis involves bacterial entry through the eustachian tube following a viral upper respiratory infection or via hematogenous spread. Staphylococcus aureus adheres to the mucosal lining of the middle ear, leading to the release of cytotoxins, inflammation, and pus formation behind the tympanic membrane.
Clinical Manifestations of Staphylococcus Acute Otitis Media
Hallmark Symptoms
- Intense otalgia (ear pain), often unilateral
- Fever (≥38°C or 100.4°F)
- Ear fullness and hearing loss
- Otorrhea (ear discharge), especially in tympanic membrane rupture
- Irritability and poor feeding in infants
In MRSA infections, symptoms may be more severe or prolonged and may fail to respond to first-line antibiotics.
Diagnostic Evaluation and Microbiological Identification
Otoscopic Examination
- Bulging, erythematous tympanic membrane
- Loss of normal light reflex
- Perforation with purulent drainage in advanced cases
Laboratory and Microbial Testing
- Ear Swab Culture (especially in otorrhea or recurrent AOM): Confirms presence of S. aureus or MRSA
- Tympanocentesis: In refractory or immunocompromised cases
- CBC and CRP: May show leukocytosis and inflammation
- Audiometry: In chronic or recurrent episodes to assess hearing impact
Treatment Protocol for Staphylococcal AOM
Antibiotic Selection
Treatment must be guided by local resistance profiles and patient-specific factors.
Methicillin-Sensitive S. aureus (MSSA)
- Amoxicillin-clavulanate
- Cephalexin
- Cefuroxime
Methicillin-Resistant S. aureus (MRSA)
- Clindamycin
- Trimethoprim-sulfamethoxazole
- Linezolid (oral)
- Vancomycin (IV for systemic involvement)
Duration
- 7–10 days for uncomplicated cases
- Up to 14 days for severe or recurrent infections
Adjunctive Therapies
- Analgesics (acetaminophen or ibuprofen)
- Decongestants (for Eustachian tube support)
- Topical antibiotics (e.g., ciprofloxacin drops for otorrhea)
- Tympanostomy tubes in recurrent cases
Complications of Untreated Staph AOM
Failure to manage staphylococcus acute otitis media can result in serious complications, particularly with MRSA strains:
- Tympanic membrane perforation
- Mastoiditis
- Facial nerve palsy
- Labyrinthitis
- Intracranial spread (meningitis, brain abscess)
Recurrent and Chronic Otitis Media Considerations
Patients with ≥3 episodes in 6 months or ≥4 in 12 months should undergo further evaluation. Contributing factors include:
- Allergies or chronic rhinosinusitis
- Eustachian tube dysfunction
- Persistent nasal staphylococcal colonization
Management may involve:
- Tympanostomy tube insertion
- Adenoidectomy
- MRSA decolonization (nasal mupirocin, chlorhexidine washes)
Prevention of Staphylococcal Ear Infections
Immunization
While no vaccine exists for S. aureus, influenza and pneumococcal vaccines help reduce AOM incidence overall.
Hygiene and Environmental Control
- Avoid secondhand smoke exposure
- Promote breastfeeding in infants (protective against AOM)
- Hand hygiene and disinfection of personal items
- Avoidance of unnecessary antibiotic use to limit resistance development
Frequently Asked Questions
How can I tell if my child has staphylococcal otitis media?
Definitive diagnosis requires culture. Clinical clues include persistent infection despite amoxicillin and presence of purulent otorrhea.
Is MRSA ear infection dangerous?
Yes. MRSA-associated AOM can cause aggressive tissue damage, systemic illness, and treatment challenges due to resistance.
Can staphylococcus cause recurrent ear infections?
Yes. Particularly in nasal carriers or those with chronic Eustachian tube dysfunction, S. aureus can contribute to recurrent AOM.
When is surgery considered?
Tympanostomy tube insertion is recommended for frequent recurrences or persistent fluid impacting hearing or development.
Staphylococcus acute otitis media, though less frequently diagnosed than other bacterial causes, poses significant risks due to its virulence and antibiotic resistance. Vigilant clinical evaluation, early identification through culture, and evidence-based antibiotic therapy are essential for optimal outcomes. For recurrent or complicated cases, a multidisciplinary approach involving ENT specialists and infectious disease consultants is often warranted. Prevention strategies and resistance control measures further support long-term patient health.