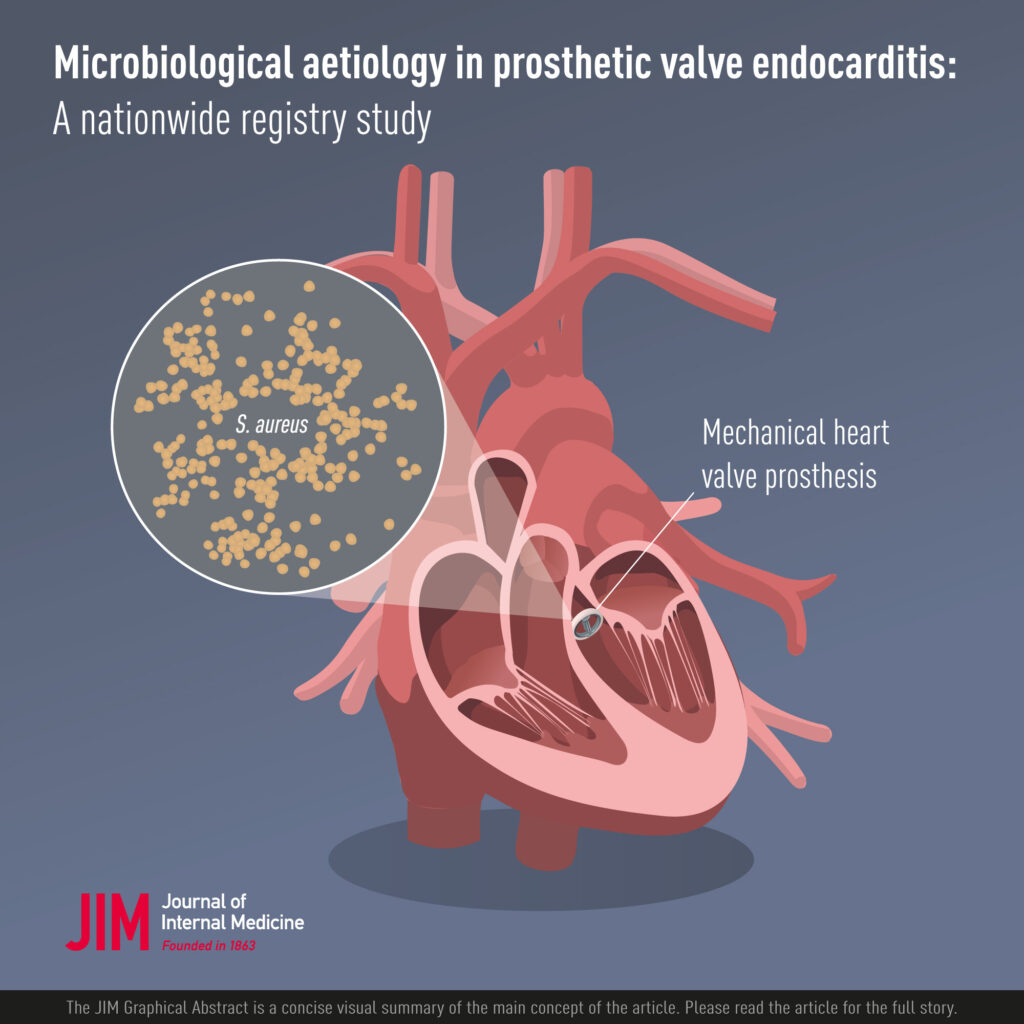
Staphylococcal prosthetic heart valve endocarditis (PVE) is a severe and complex infection that affects individuals with artificial heart valves. The most common causative agents are Staphylococcus aureus and coagulase-negative staphylococci (CoNS), including methicillin-resistant strains. The infection is characterized by microbial colonization of the prosthetic material, leading to destructive inflammation and systemic complications. Given its high morbidity and mortality rates, timely diagnosis and targeted management are critical.
Epidemiology and Classification of Staphylococcal PVE
Incidence and Risk Groups
Staphylococcal PVE accounts for up to 30% of prosthetic valve infections and carries a higher risk in the following groups:
- Patients with recent valve replacement (within 1 year)
- Immunocompromised individuals
- Hemodialysis patients
- Individuals with previous infective endocarditis
- Post-operative patients with prolonged hospital stays or indwelling catheters
Timing of Onset
PVE is classified based on the time since valve implantation:
- Early-onset PVE: Occurs within 60 days post-surgery; often nosocomial and caused by S. aureus or CoNS.
- Late-onset PVE: Manifests after 60 days; commonly due to hematogenous spread, also involving staphylococci.
Pathophysiology: Mechanisms of Prosthetic Valve Infection
Staphylococcal PVE arises when bacteria adhere to prosthetic materials and evade host defenses, forming biofilms that are resistant to antibiotics and immune clearance.
Clinical Presentation and Symptoms
Systemic and Cardiac Manifestations
The clinical features may be subtle, particularly in early-onset cases, yet progressively worsen without intervention.
- Fever and chills (may be absent in elderly or immunosuppressed)
- New or changing heart murmur
- Embolic events: stroke, pulmonary embolism, renal infarction
- Heart failure symptoms: dyspnea, fatigue, peripheral edema
- Septicemia and signs of systemic toxicity
Physical Examination Findings
- Janeway lesions, Osler nodes (rare in PVE)
- Splenomegaly
- Signs of valve dysfunction (regurgitation, stenosis)
- Neurological deficits from emboli
Diagnostic Criteria and Investigations
Modified Duke Criteria
Diagnosis of staphylococcal PVE relies on clinical, microbiological, and imaging findings. The Modified Duke Criteria include:
- Major Criteria:
- Positive blood cultures for S. aureus or CoNS in two separate samples
- Evidence of endocardial involvement via echocardiography
- Minor Criteria:
- Predisposing heart condition or IV drug use
- Fever >38°C
- Vascular or immunologic phenomena
Imaging Modalities
- Transesophageal echocardiography (TEE): Gold standard for detecting vegetations, abscesses, and prosthetic dehiscence
- CT or PET/CT scan: Useful in identifying extracardiac complications and prosthetic infections
Laboratory Studies
- Repeated blood cultures
- Elevated ESR, CRP, and procalcitonin
- CBC: Leukocytosis or anemia of chronic disease
- Renal and hepatic function tests
Antimicrobial Management of Staphylococcal PVE
Empirical Therapy
Empirical treatment should be initiated promptly and adjusted upon culture results.
Early-onset PVE:
- Vancomycin (for MRSA or CoNS)
- Rifampin (excellent biofilm penetration)
- Gentamicin (for synergy, limited duration)
Late-onset PVE:
- Nafcillin or Oxacillin for MSSA
- Vancomycin if MRSA is suspected or confirmed
Duration of Therapy
- Minimum of 6 weeks of intravenous antibiotics
- Rifampin often added after initial bacteremia is cleared
Surgical Considerations in Staph PVE
Indications for Valve Replacement
Surgical intervention is often necessary due to high rates of valve destruction and complications. Indications include:
- Uncontrolled infection despite antibiotics
- Valve dehiscence or significant regurgitation
- Recurrent embolic events
- Formation of annular abscesses
- Prosthesis dysfunction with heart failure
Surgical Approach
- Removal of infected prosthesis
- Debridement of infected tissue
- Replacement with homograft or mechanical/bioprosthetic valve
- Postoperative antibiotic therapy continuation
Complications and Prognostic Factors
Major Complications
- Sepsis and septic shock
- Cerebral infarction or hemorrhage
- Mycotic aneurysms
- Renal failure
- Heart block from abscess extension
Prognosis
The overall mortality rate ranges between 20–40%, significantly higher in MRSA cases or with delayed intervention. Prognosis improves with:
- Early diagnosis
- Prompt initiation of targeted antibiotics
- Timely surgical management
Preventive Measures and Prophylaxis
Antimicrobial Prophylaxis
- Recommended for high-risk patients undergoing dental or invasive procedures
- Single-dose amoxicillin or clindamycin in penicillin-allergic individuals
Hospital-Based Strategies
- Strict aseptic protocols in ICUs and surgical theaters
- Minimizing catheter use and prompt removal
- Routine MRSA decolonization in high-risk surgeries
Frequently Asked Questions
How is prosthetic valve endocarditis different from native valve endocarditis?
PVE often presents with subtle symptoms, involves biofilm-forming organisms, and is more resistant to therapy, requiring aggressive management and surgery more frequently.
Can staphylococcal PVE be cured without surgery?
While rare, cure without surgery is possible in selected late-onset cases with stable prosthesis and rapid microbiological clearance, but surgery remains the mainstay for most patients.
What are the long-term outcomes after PVE treatment?
Survivors often require lifelong follow-up, and recurrence risk remains elevated. Reinfection, prosthesis dysfunction, and need for reoperation are common.
Staphylococcal prosthetic heart valve endocarditis represents a formidable clinical challenge marked by aggressive infection, biofilm resistance, and high mortality. Accurate diagnosis through echocardiography and blood cultures, coupled with potent antimicrobial therapy and surgical intervention when indicated, forms the backbone of effective management. Preventive strategies remain essential to mitigate the risk in vulnerable populations and healthcare environments.

