Staphylococcal pneumonia is a serious and potentially life-threatening bacterial infection of the lungs caused by Staphylococcus aureus, including its methicillin-resistant strains (MRSA). It can present as either community-acquired or hospital-acquired pneumonia and often follows viral infections or develops in vulnerable patient populations. Due to its aggressive nature and potential for rapid progression, early diagnosis and appropriate treatment are critical.
Etiology and Pathogenesis of Staphylococcal Pneumonia
Causative Agent: Staphylococcus aureus
Staphylococcus aureus is a Gram-positive coccus that colonizes the skin and nasopharynx. It becomes pathogenic when it gains access to sterile sites, such as the alveoli, where it incites a robust inflammatory response.
Types of Strains
- Methicillin-sensitive Staphylococcus aureus (MSSA): Common in the general population.
- Methicillin-resistant Staphylococcus aureus (MRSA): Associated with worse clinical outcomes and more severe infections.
- Panton-Valentine Leukocidin (PVL)-producing strains: Linked to necrotizing pneumonia, especially in younger, previously healthy individuals.
Risk Factors and Predisposing Conditions
Several conditions increase the likelihood of developing staphylococcal pneumonia:
- Post-influenza viral infections
- Immunocompromised states (e.g., HIV, cancer)
- Mechanical ventilation or intubation
- Recent hospitalization or surgery
- Chronic lung diseases (COPD, bronchiectasis)
- Intravenous drug use
The emergence of community-associated MRSA (CA-MRSA) has expanded the at-risk population to include young and otherwise healthy individuals.
Clinical Manifestations of Staph Lung Infection
The onset of staphylococcal pneumonia may be abrupt and severe, especially in MRSA-associated cases.
Key Symptoms
- High-grade fever and chills
- Productive cough with purulent or bloody sputum
- Pleuritic chest pain
- Dyspnea and respiratory distress
- Tachypnea and hypoxia
- Signs of sepsis in advanced stages
Physical Examination Findings
- Decreased breath sounds
- Crackles or rales on auscultation
- Signs of consolidation or pleural effusion
Diagnostic Approach and Laboratory Evaluation
Accurate and timely diagnosis is vital due to the rapid progression and high mortality associated with staphylococcal pneumonia.
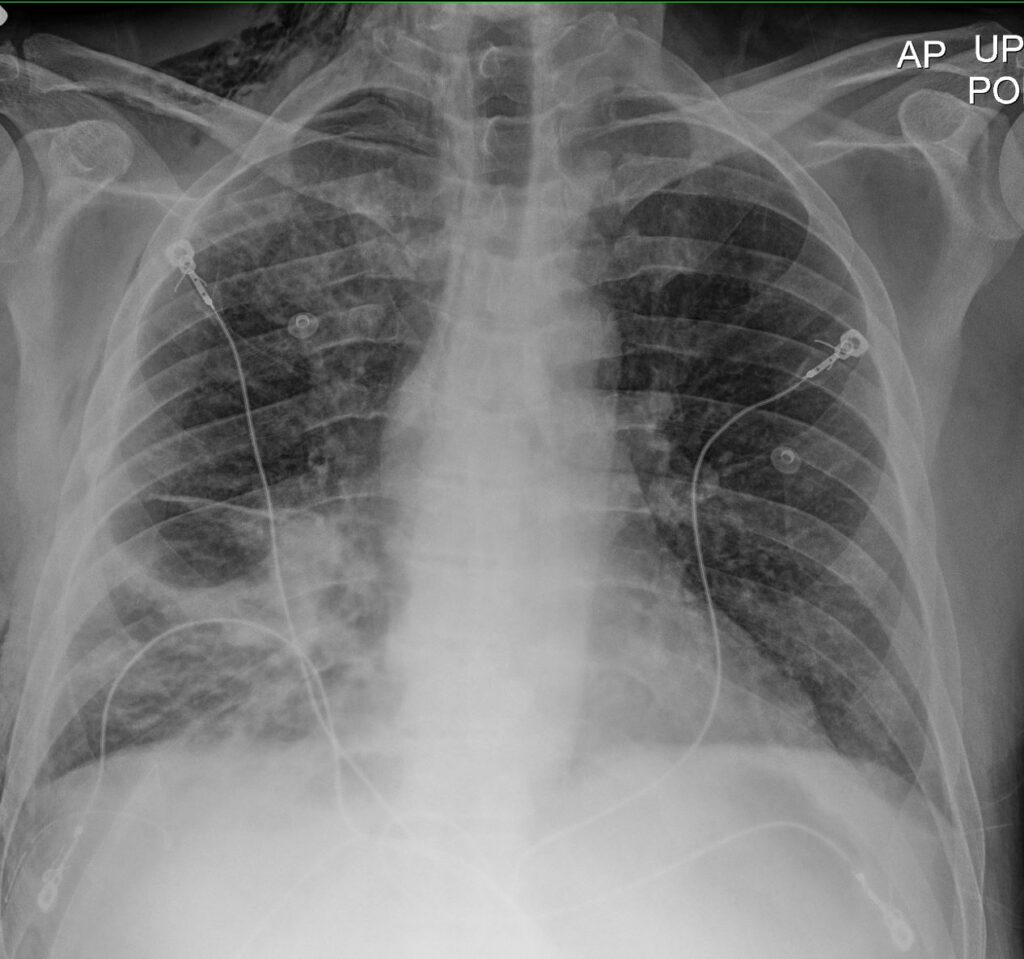
Imaging
- Chest X-ray: Shows patchy or lobar infiltrates, cavitation, and abscess formation.
- CT scan: Offers detailed assessment of necrosis and empyema.
Microbiological Testing
- Sputum culture and Gram stain
- Blood cultures
- Bronchoalveolar lavage (BAL) in intubated patients
- PCR and molecular assays for rapid MRSA detection
Laboratory Tests
- CBC: Elevated white blood cell count with neutrophilia
- Inflammatory markers: Elevated CRP and procalcitonin
- Arterial blood gases (ABG): Assess severity of hypoxia
Management of Staphylococcal Pneumonia
Antimicrobial Therapy
Initiation of empirical antibiotic therapy is critical and should be tailored upon microbiological confirmation.
MSSA Infections
- Nafcillin or Oxacillin
- Cefazolin
- Clindamycin in penicillin-allergic patients
MRSA Infections
- Vancomycin (first-line agent)
- Linezolid (better lung penetration, oral option)
- Ceftaroline (a fifth-generation cephalosporin with MRSA activity)
Combination therapy may be necessary in severe cases, especially if septic shock or empyema is present.
Supportive Care
- Oxygen supplementation
- IV fluids and vasopressors for septic shock
- Mechanical ventilation if respiratory failure develops
- Drainage of pleural effusion or abscess if indicated
Complications and Prognostic Considerations
Major Complications
- Necrotizing pneumonia
- Pulmonary abscess
- Empyema
- Septicemia and septic shock
- Acute respiratory distress syndrome (ARDS)
- Multiorgan dysfunction syndrome (MODS)
Mortality rates can be high, particularly in MRSA cases or in patients with delayed treatment or underlying comorbidities.
Preventive Strategies and Public Health Implications
Hospital Infection Control
- Strict hand hygiene practices
- Use of contact precautions for MRSA-positive patients
- Regular decontamination of medical equipment
Vaccination and Antiviral Measures
- Influenza vaccination to reduce post-viral bacterial pneumonia
- Pneumococcal vaccine for differential protection
MRSA Decolonization
- Mupirocin nasal ointment and chlorhexidine washes in recurrent carriers or pre-surgical patients
Frequently Asked Questions
How is staphylococcal pneumonia different from other bacterial pneumonias?
Staphylococcal pneumonia often presents more aggressively, with necrotic lung lesions and systemic involvement. MRSA strains pose greater therapeutic challenges due to antibiotic resistance.
Is staphylococcal pneumonia contagious?
Yes. It can spread via respiratory droplets or contaminated surfaces. Isolation protocols are recommended in healthcare settings.
What is the prognosis for staphylococcal pneumonia?
With timely diagnosis and appropriate antibiotics, the prognosis is favorable in MSSA cases. MRSA and necrotizing forms are associated with higher morbidity and mortality.
Can staphylococcal pneumonia recur?
Yes. Particularly in individuals with unresolved colonization, immunosuppression, or inadequate initial treatment.
Staphylococcal pneumonia remains a significant cause of morbidity and mortality, especially in hospital settings and among immunocompromised individuals. Prompt recognition, empirical antibiotic initiation, and targeted therapy based on culture results are paramount. Preventive measures and rigorous infection control practices are essential to limit the spread of MRSA and improve patient outcomes.

