Squamous cell carcinoma (SCC) of the vulva is the most common type of vulvar cancer, arising from the squamous epithelium of the external female genitalia. Though relatively rare compared to other gynecological malignancies, its incidence is rising, particularly among older women and those infected with high-risk strains of human papillomavirus (HPV). This comprehensive guide outlines the key factors contributing to vulvar SCC, its clinical manifestations, diagnostic workup, therapeutic options, and preventive measures.

Understanding Vulvar Squamous Cell Carcinoma
Squamous cell carcinoma of the vulva originates from the flat, scale-like cells lining the surface of the vulvar skin. It accounts for approximately 90% of all vulvar cancers. The disease typically affects the labia majora or minora but can also involve the clitoris or perineal region. Vulvar SCC develops through two major pathways: one associated with HPV infection and the other related to chronic inflammatory dermatoses, such as lichen sclerosus.
Risk Factors for Vulvar Squamous Cell Carcinoma
Human Papillomavirus (HPV) Infection
Persistent infection with high-risk HPV strains, especially HPV-16, is a well-documented risk factor for vulvar SCC. HPV-related SCC tends to affect younger women and often arises from vulvar intraepithelial neoplasia (VIN).
Chronic Inflammatory Skin Disorders
Non-HPV vulvar SCC is more prevalent in older women and is often associated with conditions like lichen sclerosus and lichen planus, which cause chronic inflammation and epithelial thinning.
Immunosuppression
Women with compromised immune systems, including those with HIV or organ transplant recipients on immunosuppressive therapy, have a higher risk of developing vulvar SCC due to impaired clearance of HPV and precancerous cells.
Smoking
Tobacco use is linked to both HPV-related and independent SCC by promoting carcinogenic changes in the vulvar epithelium.
Age and Genetics
The risk of vulvar SCC increases significantly with age, particularly in women over 65. While rare, genetic predispositions, such as mutations in tumor suppressor genes, may play a role.
Clinical Presentation: Recognizing Symptoms of Vulvar SCC
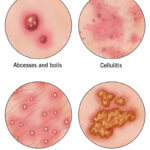
Vulvar SCC often develops slowly, making early detection critical. Symptoms may include:
- Persistent vulvar itching, burning, or discomfort
- A visible lump, ulcer, or wart-like lesion
- Skin thickening, discoloration, or scaling
- Pain during urination or intercourse
- Foul-smelling discharge or bleeding unrelated to menstruation
Lesions are typically located on the labia majora and may appear red, white, or pigmented. As the tumor progresses, it may invade surrounding tissues, including the urethra, vagina, or anus.
Diagnostic Evaluation of Vulvar Squamous Cell Carcinoma
Clinical Examination
A thorough gynecologic examination is essential. Any suspicious lesion should be evaluated, particularly those resistant to topical treatments or those with atypical pigmentation, ulceration, or induration.
Biopsy
Histologic confirmation is mandatory for diagnosis. A punch biopsy or incisional biopsy under local anesthesia is performed to assess cellular atypia, depth of invasion, and tumor type.
Imaging Studies
Once invasive SCC is diagnosed, imaging may be required to assess the extent of disease:
- Pelvic MRI: Evaluates local invasion
- CT Scan or PET-CT: Detects lymph node involvement and distant metastasis
- Ultrasound: Assesses inguinal lymph nodes
Staging and Classification of Vulvar SCC
The FIGO staging system is used for vulvar cancers, based on the size of the primary tumor, depth of stromal invasion, and spread to lymph nodes or distant organs.
- Stage I: Confined to the vulva/perineum
- Stage II: Adjacent spread (e.g., lower urethra, vagina, anus)
- Stage III: Lymph node involvement
- Stage IV: Distant metastasis
Prognosis strongly correlates with the stage at diagnosis. Early-stage SCC has a high cure rate, whereas advanced disease carries a worse prognosis due to regional or systemic spread.
Treatment Strategies for Vulvar Squamous Cell Carcinoma
Surgical Management
Wide Local Excision
For small, localized tumors, wide local excision with clear margins is often sufficient and minimizes disfigurement.
Radical Vulvectomy
In more extensive disease, partial or total radical vulvectomy may be necessary. Reconstruction techniques can be employed for functional and aesthetic restoration.
Sentinel Lymph Node Biopsy or Lymphadenectomy
Assessment of lymph node status is crucial. Sentinel lymph node biopsy is preferred in early-stage disease to reduce complications. In cases of nodal involvement, a full inguinofemoral lymphadenectomy may be warranted.
Radiation Therapy
Adjuvant or primary radiation therapy is used in cases with positive margins, nodal involvement, or inoperable tumors. Intensity-modulated radiotherapy (IMRT) allows for precise targeting while sparing surrounding tissues.
Chemoradiation
Concurrent chemotherapy with agents such as cisplatin may be used with radiation for locally advanced or recurrent disease, improving response rates and survival outcomes.
Follow-Up and Surveillance
Long-term follow-up is critical, as recurrence occurs in up to 30% of patients. Surveillance typically includes:
- Physical examination every 3 to 6 months for the first 2 years, then annually
- Imaging as indicated for suspicious symptoms or signs
- HPV testing and counseling when appropriate
Patients should be educated on self-examination, symptom recognition, and the importance of prompt medical evaluation for any changes.
Prevention and Risk Reduction
HPV Vaccination
Vaccination against HPV, particularly before the onset of sexual activity, significantly reduces the risk of developing HPV-related vulvar SCC.
Smoking Cessation
Quitting tobacco use decreases vulvar cancer risk and improves overall gynecologic health.
Management of Precursor Lesions
Early treatment of VIN and chronic inflammatory dermatoses with topical corticosteroids, immunomodulators, or surgical excision can prevent progression to invasive SCC.
Regular Gynecologic Exams
Routine pelvic exams and early biopsy of suspicious vulvar changes are vital for early diagnosis and improved prognosis.
Frequently Asked Questions
What is the survival rate for vulvar squamous cell carcinoma?
The 5-year survival rate exceeds 85% for early-stage disease. Advanced stages with lymph node involvement have a significantly lower survival rate, around 50–60%.
Can vulvar SCC return after treatment?
Yes, recurrence is possible, especially within the first two years post-treatment. Close follow-up is essential for early detection of recurrence.
Is vulvar SCC painful?
Pain is not always present in early stages but may develop as the tumor enlarges, ulcerates, or invades nearby structures.
Is vulvar SCC contagious?
No, the cancer itself is not contagious. However, the HPV infection associated with some cases of vulvar SCC is sexually transmissible.
Squamous cell carcinoma of the vulva is a serious but treatable malignancy when identified early. Through a clear understanding of its risk factors, clinical manifestations, diagnostic tools, and evidence-based treatments, we can improve patient outcomes and reduce disease burden. Preventive strategies, including HPV vaccination and routine gynecologic care, remain essential components of public health efforts to combat vulvar cancer.