Small lymphocytic lymphoma (SLL) is an indolent B-cell non-Hodgkin lymphoma (NHL) that is biologically and clinically similar to chronic lymphocytic leukemia (CLL). These two conditions are considered different manifestations of the same disease entity—distinguished mainly by the location of the abnormal lymphocytes. While CLL primarily affects the blood and bone marrow, SLL manifests predominantly in the lymph nodes and other lymphoid tissues.
Understanding Small Lymphocytic Lymphoma
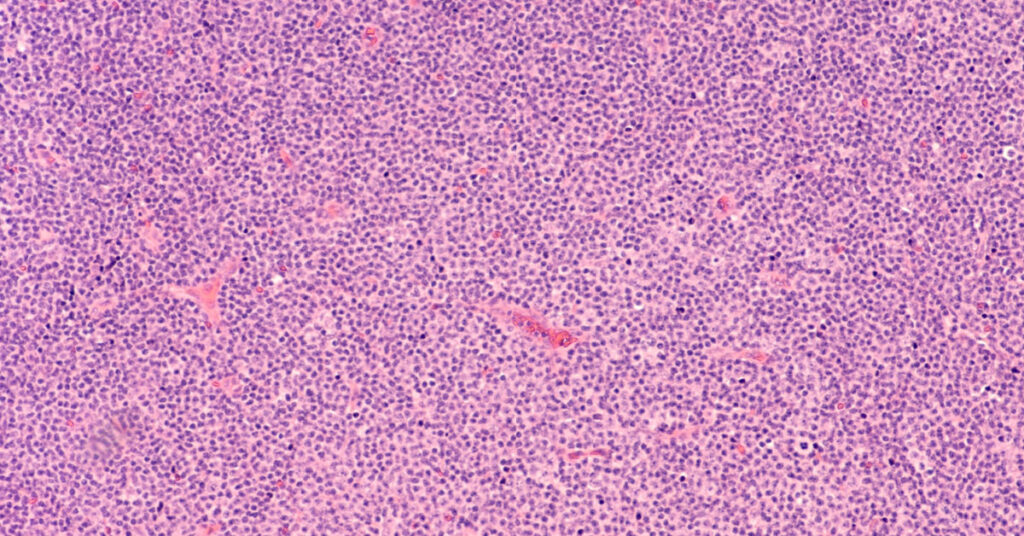
SLL arises from mature B lymphocytes and is characterized by the slow proliferation of small, round lymphocytes that infiltrate lymphoid structures. The disease progresses gradually, often without symptoms for extended periods, but it can eventually lead to significant lymphadenopathy and immune dysfunction.
SLL and CLL: Two Faces of the Same Disease
| Feature | SLL | CLL |
|---|---|---|
| Primary Site | Lymph nodes, spleen | Blood, bone marrow |
| Blood Lymphocyte Count | <5,000/µL | ≥5,000/µL |
| Bone Marrow Involvement | Variable | Common |
| Clinical Management | Largely overlapping | Largely overlapping |
| WHO Classification | One disease entity (CLL/SLL) | One disease entity (CLL/SLL) |
Risk Factors and Etiology of SLL
The exact cause of small lymphocytic lymphoma remains unknown, but several factors increase the likelihood of developing the disease:
- Age: Most patients are over 60 years old.
- Sex: Slight male predominance.
- Family History: Increased risk with a first-degree relative who has CLL/SLL.
- Environmental Exposures: Some data suggest links to pesticides, herbicides, and other chemical agents.
- Genetic Mutations: Aberrations such as deletions at 13q, 11q, and 17p, and trisomy 12 are associated with SLL progression and prognosis.
Clinical Presentation and Symptoms of SLL
SLL often presents with painless, persistent lymphadenopathy. Symptoms may be absent in the early stages, making diagnosis incidental in many cases.
Common Symptoms:
- Swollen lymph nodes in the neck, armpit, or groin
- Splenomegaly and hepatomegaly
- Night sweats
- Fatigue
- Unexplained weight loss
- Frequent infections due to immune suppression
B symptoms (fever, weight loss, night sweats) typically indicate disease progression or transformation into a more aggressive lymphoma, such as Richter’s transformation.
Diagnostic Evaluation of Small Lymphocytic Lymphoma
Imaging and Laboratory Tests
- CT scan or PET-CT: To assess nodal involvement and organomegaly
- Complete Blood Count (CBC): Often normal in SLL, distinguishing it from CLL
- Flow Cytometry: Detects clonal B-cell population; key in differentiating SLL/CLL from other lymphomas
- Bone Marrow Biopsy: May be required in staging or in cases with suspected transformation
Immunophenotype
Characteristic immunophenotypic profile includes:
- CD19⁺, CD20⁺ (dim), CD5⁺, CD23⁺
- Light chain restriction (kappa or lambda)
- Low surface immunoglobulin expression
Staging of Small Lymphocytic Lymphoma
Unlike Hodgkin lymphoma, SLL follows the Ann Arbor staging system used for non-Hodgkin lymphomas:
- Stage I: Involvement of a single lymph node region or a single extralymphatic site
- Stage II: Two or more lymph node regions on the same side of the diaphragm
- Stage III: Lymph node involvement on both sides of the diaphragm
- Stage IV: Diffuse or disseminated involvement of one or more extralymphatic organs
Treatment Options for SLL
Treatment decisions depend on disease stage, patient age, performance status, and the presence of symptoms. Asymptomatic patients with early-stage SLL may be managed with active surveillance.
First-Line Therapies
- Chemoimmunotherapy:
- FCR: Fludarabine, Cyclophosphamide, Rituximab
- BR: Bendamustine, Rituximab
- Targeted Therapies:
- BTK inhibitors: Ibrutinib, Acalabrutinib
- BCL-2 inhibitors: Venetoclax (often with Obinutuzumab)
- PI3K inhibitors: Idelalisib (in select cases)
Second-Line and Salvage Therapies
- Alternate BTK inhibitors or BCL-2 inhibitors after resistance or intolerance
- Enrollment in clinical trials exploring CAR T-cell therapy or novel agents
Management of Complications
- Richter’s Transformation: High-grade transformation requiring aggressive chemotherapy
- Autoimmune Cytopenias: Often require corticosteroids or immunosuppressive therapy
Prognosis and Survival in SLL
SLL is considered incurable but highly manageable. Many patients live for years with minimal symptoms.
| Prognostic Factor | Impact |
|---|---|
| 17p deletion or TP53 mutation | Poor prognosis, reduced therapy response |
| IGHV mutation status | Unmutated = more aggressive |
| Beta-2 microglobulin levels | Elevated = worse outcomes |
| Performance status | Influences therapy tolerance |
Median survival ranges from 8 to 15 years, depending on genetic and clinical features.
Frequently Asked Questions:
Is small lymphocytic lymphoma the same as CLL?
SLL and CLL are considered manifestations of the same disease. The distinction lies in the location of abnormal B cells—lymph nodes vs blood.
What is the main treatment for SLL?
Initial treatment may include chemoimmunotherapy or targeted therapies. Asymptomatic patients are often monitored without treatment.
Can SLL transform into aggressive lymphoma?
Yes. Approximately 5–10% of cases undergo Richter’s transformation into diffuse large B-cell lymphoma (DLBCL), which requires more intensive treatment.
How is SLL diagnosed?
Diagnosis is confirmed through lymph node biopsy, flow cytometry, and immunophenotyping to distinguish it from other lymphoproliferative disorders.
Is SLL hereditary?
There is a familial predisposition, particularly in those with relatives diagnosed with SLL or CLL, but no direct inheritance pattern has been established.
Small lymphocytic lymphoma is a slow-growing, yet clinically significant B-cell lymphoma closely related to CLL. Early recognition, precise diagnosis through immunophenotyping, and personalized treatment approaches are essential to improve outcomes. Advances in targeted therapy have redefined management paradigms, offering prolonged disease control and improved quality of life.