Small cell lung carcinoma (SCLC) is a highly aggressive form of lung cancer characterized by rapid growth and early metastasis. Accounting for approximately 10–15% of all lung cancers, SCLC is strongly associated with tobacco exposure and is known for its neuroendocrine characteristics and high proliferative index. Despite being responsive to chemotherapy and radiotherapy, SCLC often relapses, making long-term survival a significant clinical challenge.
Classification and Staging of Small Cell Lung Carcinoma
SCLC is traditionally classified based on the extent of disease spread, with staging playing a critical role in treatment planning and prognosis.
Limited-Stage SCLC
- Cancer is confined to one hemithorax and can be treated within a single radiation field.
- May include ipsilateral mediastinal and supraclavicular lymph nodes.
- Represents approximately 30% of cases at diagnosis.
Extensive-Stage SCLC
- Cancer has spread beyond one hemithorax or to distant organs (e.g., liver, bone, brain).
- Includes malignant pleural effusion or contralateral thoracic spread.
- Represents roughly 70% of SCLC cases upon detection.
TNM Staging System
While the limited/extensive system is most commonly used, the TNM staging classification is increasingly applied for clinical trials and treatment refinement.
Risk Factors and Etiology
Primary Risk Factor: Tobacco Use
- Over 95% of SCLC cases are linked to active or past smoking.
- Risk increases with duration and intensity of tobacco exposure.
Additional Risk Factors
- Occupational exposures (e.g., radon, asbestos, arsenic)
- Genetic predisposition and family history of lung cancer
- Secondhand smoke exposure
- Chronic obstructive pulmonary disease (COPD)
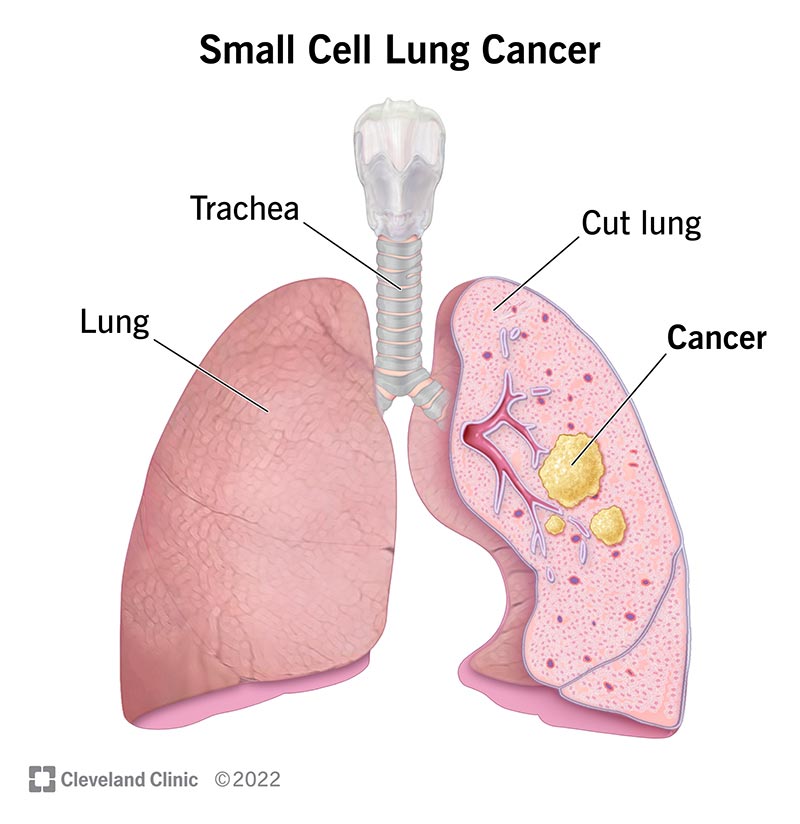
Pathophysiology and Tumor Biology
SCLC originates from neuroendocrine cells in the bronchial epithelium. It is characterized by:
- High mitotic index
- Expression of neuroendocrine markers (e.g., chromogranin A, synaptophysin)
- Frequent genetic alterations such as TP53 and RB1 mutations
- Early lymphovascular invasion and metastasis
Common Symptoms of Small Cell Lung Carcinoma
Due to its aggressive nature, symptoms of SCLC often present rapidly and are related to both primary tumor growth and metastatic spread.
Primary Lung Symptoms:
- Persistent cough
- Hemoptysis (coughing up blood)
- Dyspnea (shortness of breath)
- Chest pain
- Wheezing
Systemic and Paraneoplastic Symptoms:
- Weight loss and anorexia
- Fatigue
- Hyponatremia due to SIADH (Syndrome of Inappropriate Antidiuretic Hormone)
- Cushing’s syndrome from ectopic ACTH production
- Lambert-Eaton myasthenic syndrome (LEMS)
Diagnostic Approach
Early diagnosis is essential for optimal treatment planning. A combination of imaging, pathology, and molecular testing is used.
Imaging Techniques
- Chest CT scan with contrast (first-line imaging)
- PET-CT scan to assess metastatic spread
- MRI of the brain (due to frequent brain metastasis)
- Bone scans if skeletal symptoms are present
Histological Confirmation
Tissue biopsy via:
- Bronchoscopy with transbronchial biopsy
- CT-guided needle biopsy
- Pleural fluid cytology (if effusion is present)
Immunohistochemistry Markers:
- Positive for CD56, chromogranin A, synaptophysin
- High Ki-67 proliferative index (>50%)
Treatment Strategies for SCLC
Treatment is stage-dependent and aims for remission in limited-stage disease or palliation and survival extension in extensive-stage disease.
Limited-Stage SCLC
- Concurrent Chemoradiation (etoposide + cisplatin or carboplatin)
- Thoracic radiotherapy administered early
- Prophylactic Cranial Irradiation (PCI) to reduce brain metastasis risk
- Surgery is rare, considered only in very early-stage tumors (T1-2, N0)
Extensive-Stage SCLC
- Chemotherapy (etoposide + carboplatin/cisplatin) is the cornerstone
- Immunotherapy (e.g., atezolizumab, durvalumab) added to first-line regimens
- Palliative radiotherapy for symptomatic metastases
- Whole-brain radiotherapy (WBRT) for brain metastasis
- Clinical trials may provide access to novel agents
Prognosis and Survival Outcomes
SCLC has a poor prognosis due to its aggressive biology and early metastasis.
| Stage | Median Survival | 2-Year Survival Rate |
|---|---|---|
| Limited Stage | 15–20 months | 20–25% |
| Extensive Stage | 8–13 months | <5% |
- Brain, liver, and bone metastases significantly reduce survival
- Recurrence is common within months of initial treatment
Research and Emerging Therapies
Ongoing research targets the unique biology of SCLC through:
- PARP inhibitors (targeting DNA repair pathways)
- Checkpoint inhibitors (expanding beyond PD-L1 axis)
- DLL3-targeted therapies (e.g., Rova-T, under development)
- Tumor vaccines and cellular therapies
Biomarker-driven studies and genomic profiling are becoming more central to personalized treatment approaches.
Frequently Asked Questions:
Is small cell lung carcinoma curable?
Limited-stage SCLC may be curable with aggressive treatment, but extensive-stage disease is generally not curable, only manageable.
How is SCLC different from non-small cell lung cancer?
SCLC grows and spreads faster, is more responsive to chemotherapy and radiation, and has a worse prognosis.
Can non-smokers develop SCLC?
It is extremely rare, but possible. The overwhelming majority of cases are linked to smoking.
What are the first signs of SCLC?
Common early symptoms include persistent cough, chest pain, and shortness of breath. Neurological symptoms may indicate brain metastases.
How often should high-risk individuals be screened?
Annual low-dose CT scans are recommended for individuals aged 50–80 with a significant smoking history.
Small cell lung carcinoma is an aggressive and often rapidly fatal malignancy that demands early recognition and prompt, coordinated intervention. Although initial responsiveness to treatment is high, the disease frequently recurs. Continued advancements in immunotherapy, molecular research, and targeted treatments are vital to improving long-term outcomes for affected patients.

very informative articles or reviews at this time.