Sleep-onset insomnia, also referred to as initial insomnia, is a common sleep disorder defined by difficulty initiating sleep at bedtime. Despite sufficient opportunity and a conducive environment for rest, individuals with this condition find themselves unable to fall asleep within a typical timeframe, often taking more than 30 minutes to do so. The disorder affects people across all age groups and significantly impairs daytime functioning, cognitive clarity, and emotional stability.

Understanding Sleep-Onset Insomnia
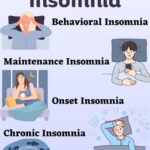
Sleep-onset insomnia is categorized under chronic insomnia disorder when symptoms persist for at least three nights a week over three months. It may occur independently or in conjunction with other forms of insomnia, such as sleep maintenance or early-morning awakening insomnia. The hallmark feature is delayed sleep latency — the time taken to transition from wakefulness to sleep.
Diagnostic Criteria:
- Prolonged sleep latency (>30 minutes)
- Sleep difficulties present at least three times per week
- Symptoms last for more than three months
- Daytime distress or functional impairment due to poor sleep
Common Causes of Sleep-Onset Insomnia
1. Psychological Stress and Anxiety
Heightened mental activity, worry, or racing thoughts activate the hypothalamic-pituitary-adrenal (HPA) axis, increasing arousal and delaying sleep onset. Performance anxiety regarding sleep itself — also known as psychophysiological insomnia — is common.
2. Poor Sleep Hygiene
Inconsistent sleep schedules, late-night screen exposure, excessive napping, and stimulant intake (caffeine, nicotine) impair circadian alignment and inhibit melatonin secretion, prolonging sleep latency.
3. Circadian Rhythm Disorders
Delayed sleep-wake phase disorder (DSWPD) is commonly associated with sleep-onset insomnia. It occurs when the internal body clock is misaligned with the desired bedtime.
4. Substance Use
Stimulants like caffeine, decongestants, energy drinks, and some antidepressants delay the onset of sleep. Alcohol may induce sleepiness initially but leads to fragmented sleep later in the night.
5. Chronic Pain or Medical Conditions
Conditions such as arthritis, GERD, and migraines can prevent individuals from falling asleep comfortably.
6. Neurological and Psychiatric Disorders
ADHD, bipolar disorder, and PTSD are often accompanied by sleep disturbances, including delayed sleep onset.
Symptoms and Effects of Sleep-Onset Insomnia
- Difficulty falling asleep despite adequate time in bed
- Heightened pre-sleep arousal (both cognitive and somatic)
- Clock-watching and frustration around bedtime
- Fatigue, irritability, poor concentration, and memory problems during the day
- Negative sleep-related beliefs reinforcing insomnia patterns
Diagnostic Approaches
1. Sleep Diary
A 1–2 week log tracking sleep patterns, bedtime rituals, latency, and wake times provides a foundation for clinical assessment.
2. Actigraphy
Wearable activity monitors offer objective data on sleep-wake cycles, particularly useful in identifying circadian rhythm disturbances.
3. Clinical Interview
A structured review of lifestyle, mental health status, medications, and environmental factors helps identify contributing elements.
4. Polysomnography
Recommended when sleep-onset insomnia may be linked with other disorders, such as periodic limb movements or narcolepsy.
Treatment of Sleep-Onset Insomnia
1. Cognitive Behavioral Therapy for Insomnia (CBT-I)
CBT-I is the gold standard treatment for sleep-onset insomnia. It addresses the behavioral and cognitive factors that perpetuate difficulty falling asleep.
Core Techniques:
- Stimulus Control: Strengthens the bed-sleep association by limiting bedroom activities
- Sleep Restriction Therapy: Reduces time in bed to increase sleep drive and efficiency
- Cognitive Restructuring: Challenges maladaptive beliefs about sleep (e.g., “I must fall asleep in 10 minutes”)
- Relaxation Techniques: Guided imagery, diaphragmatic breathing, and progressive muscle relaxation to ease pre-sleep tension
2. Chronotherapy and Light Therapy
Chronotherapy gradually delays or advances bedtime to reset the internal body clock, while bright light exposure in the morning reinforces circadian alignment.
3. Melatonin Supplementation
Timed melatonin (0.5–3 mg) taken in the evening can facilitate sleep onset, especially in cases of DSWPD. It must be administered under professional guidance to avoid timing errors.
4. Pharmacological Options
Short-term use of medications may be appropriate in select cases when CBT-I is inaccessible or ineffective. These include:
- Z-drugs (zolpidem, zaleplon): Rapid-onset hypnotics with minimal hangover effects
- Low-dose doxepin: Particularly effective in elderly patients
- Melatonin agonists (ramelteon): Mimic natural melatonin and enhance circadian regulation
Sedative-hypnotics are not a long-term solution due to risks of dependence, tolerance, and rebound insomnia.
5. Lifestyle and Environmental Modifications
- Establishing consistent bed and wake times
- Reducing blue light exposure 1–2 hours before bedtime
- Avoiding stimulants after midday
- Creating a quiet, dark, cool sleep environment
- Engaging in regular aerobic exercise (early in the day)
Prevention of Recurrence
- Maintain a structured wind-down routine every night
- Address sources of stress through mindfulness or therapy
- Use the bedroom exclusively for sleep and intimacy
- Limit naps to under 30 minutes before 3 PM
- Refrain from checking the clock during the night
When to Consult a Sleep Specialist
- Symptoms persist for over three months
- Functional impairment despite lifestyle changes
- Coexisting conditions such as depression, anxiety, or chronic illness
- Need for medication evaluation or advanced therapy like CBT-I
Sleep-onset insomnia significantly disrupts the ability to initiate sleep and maintain restorative rest. By identifying its multifactorial causes and applying targeted behavioral and therapeutic interventions, long-term resolution is achievable. Evidence consistently supports cognitive-behavioral therapy as the most effective solution, offering both immediate relief and sustained improvements without pharmacological dependency.