Streptococcus pyogenes (Group A Streptococcus, or GAS) is a highly pathogenic bacterium responsible for a wide spectrum of infections, including severe skin and soft tissue infections. These infections can range from mild superficial conditions, such as impetigo, to severe, life-threatening diseases like necrotizing fasciitis.
Due to its ability to produce various virulence factors, S. pyogenes poses a significant clinical challenge. This article provides a comprehensive understanding of the types, causes, clinical presentations, and treatment protocols for Streptococcus pyogenes infections in the skin and soft tissues.
Epidemiology of Streptococcus pyogenes Skin Infections
Skin and soft tissue infections caused by Streptococcus pyogenes remain a major global health issue, with an estimated 10-15 million cases annually. Although these infections are common in community settings, they can also occur in healthcare environments, especially among immunocompromised patients or those with chronic diseases.
At-Risk Populations:
- Children and the elderly: Especially vulnerable to both mild and severe forms of infection.
- Individuals with chronic skin conditions: Such as eczema or diabetic foot ulcers.
- Patients with weakened immune systems: Including those undergoing chemotherapy or organ transplantation.
- Individuals with compromised circulation or lymphedema: At higher risk for cellulitis and other deep tissue infections.
Clinical Manifestations of Streptococcus pyogenes Infections
Streptococcus pyogenes can cause various skin infections, each with distinct characteristics. Early recognition of symptoms is essential for effective treatment.
1. Impetigo
Impetigo is one of the most common infections in children, marked by honey-colored crusts that form over fluid-filled blisters. It typically affects exposed areas, such as the face, arms, and legs, and can be highly contagious.
2. Erysipelas
Erysipelas is a superficial skin infection characterized by raised, red, and well-demarcated plaques, often on the face or legs. The infection typically presents with systemic symptoms such as fever and chills.
3. Cellulitis
Cellulitis, a deeper soft tissue infection, manifests as redness, warmth, and swelling. The skin may be tender to touch, and the borders of the infection are often less well-defined compared to erysipelas.
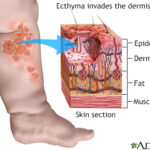
4. Necrotizing Fasciitis
Necrotizing fasciitis is a rapidly progressing soft tissue infection that causes severe pain, necrosis, and systemic toxicity. It often affects the extremities and requires immediate surgical intervention and intravenous antibiotics. Mortality rates for this condition can be high if treatment is delayed.
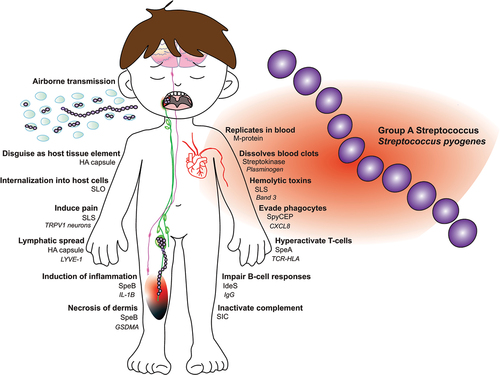
Virulence Factors of Streptococcus pyogenes
The ability of Streptococcus pyogenes to cause skin infections lies in its complex array of virulence factors. These factors contribute to the bacterium’s ability to invade tissues, evade the immune system, and cause extensive damage.
Key Virulence Factors:
- M Protein: Involved in immune evasion by preventing phagocytosis.
- Streptolysins: Toxic proteins that lyse host cells, contributing to tissue damage.
- Exotoxins (SpeA, SpeB): Superantigens that can trigger toxic shock syndrome and necrotizing fasciitis.
- Hyaluronidase and Streptokinase: Enzymes that break down connective tissue, aiding in bacterial spread.
Diagnostic Evaluation of Streptococcus pyogenes Infections
The diagnosis of Streptococcus pyogenes infections involves a combination of clinical assessment, laboratory tests, and microbiological cultures.
1. Clinical Evaluation:
A thorough clinical examination can help identify common signs such as redness, swelling, tenderness, and the presence of blisters or pustules. Systemic symptoms, including fever, chills, and hypotension, suggest more severe infections like necrotizing fasciitis or streptococcal toxic shock syndrome.
2. Laboratory Testing:
- Blood Cultures: Essential in cases of bacteremia or suspected sepsis.
- Wound Culture: Swabs from infected tissue or drainage can confirm the presence of S. pyogenes.
- Imaging Studies: X-rays, CT scans, or MRI may be used to evaluate deeper tissue involvement, especially in cases of necrotizing fasciitis.
3. Histopathology:
In severe cases, a tissue biopsy can provide additional information on the extent of necrosis and the bacterial load.
Treatment Strategies for Streptococcus pyogenes Skin Infections
Treatment of Streptococcus pyogenes infections typically involves antibiotics, surgical debridement for severe cases, and supportive care. Early intervention is crucial to reduce morbidity and mortality.
Antibiotic Therapy:
The treatment regimen depends on the severity of the infection and the clinical condition of the patient.
| Infection Type | First-Line Antibiotics | Alternative Therapy (Penicillin Allergy) |
|---|---|---|
| Impetigo | Oral penicillin or amoxicillin | Cephalexin or clindamycin |
| Erysipelas | IV penicillin G or cefazolin | Clindamycin or vancomycin |
| Cellulitis | IV cefazolin or clindamycin | Clindamycin or vancomycin |
| Necrotizing Fasciitis | IV penicillin + clindamycin | IV meropenem + vancomycin |
In severe cases of necrotizing fasciitis, surgical debridement is often required to remove necrotic tissue, along with broad-spectrum antibiotic therapy until culture results are available.
Preventing Streptococcus pyogenes Skin Infections
Prevention of Streptococcus pyogenes infections requires a multifaceted approach, particularly for individuals at high risk.
Preventive Measures Include:
- Hygiene and Skin Care: Regular handwashing and proper wound care can prevent bacterial colonization.
- Chronic Condition Management: Good management of chronic diseases, such as diabetes and vascular insufficiency, reduces the risk of infection.
- Prophylactic Antibiotics: For patients with recurrent skin infections, prophylactic antibiotic therapy may be recommended.
- Vaccination Research: Although no vaccine is currently available for S. pyogenes, research into vaccine development is ongoing.
Prognosis and Complications of Streptococcus pyogenes Infections
With timely and appropriate treatment, most skin infections caused by Streptococcus pyogenes resolve without complications. However, delay in diagnosis or treatment can result in severe outcomes.
Potential Complications:
- Sepsis: Can occur if the infection enters the bloodstream.
- Toxic Shock Syndrome (TSS): A life-threatening condition caused by the release of exotoxins.
- Chronic Ulcers: May occur in cases with delayed treatment or underlying health conditions.
- Post-Streptococcal Sequelae: Including rheumatic fever and glomerulonephritis.
Emerging Treatments and Future Research Directions
Advancements in molecular diagnostics, vaccine development, and antibiotic therapies are expected to improve outcomes for patients with Streptococcus pyogenes infections.
Promising Areas of Research:
- Rapid PCR-based diagnostics to detect S. pyogenes in wounds and blood samples.
- Monoclonal antibody therapies targeting streptococcal toxins.
- Vaccine development to prevent infections caused by S. pyogenes, particularly in high-risk populations.
Streptococcus pyogenes is a major pathogen responsible for a wide range of skin and soft tissue infections. By recognizing the clinical signs, understanding the pathogen’s virulence factors, and providing timely treatment, healthcare providers can effectively manage and reduce the impact of these infections. As research continues to evolve, the hope for improved diagnostics and preventive measures remains a key focus in the fight against Streptococcus pyogenes infections.