Staphylococcus species, primarily Staphylococcus aureus, are the leading causative agents of skin and skin structure infections (SSSIs). These gram-positive cocci, including both methicillin-sensitive (MSSA) and methicillin-resistant (MRSA) strains, are responsible for a wide spectrum of infections, ranging from superficial folliculitis to life-threatening necrotizing fasciitis.
Due to their virulence factors, adaptability, and resistance potential, Staphylococcus infections require timely diagnosis and appropriate therapy to avoid complications such as systemic dissemination, abscess formation, and osteomyelitis.
Epidemiology and Risk Factors for Staphylococcal SSSI
Staphylococcus aureus colonizes the skin, anterior nares, and mucous membranes of approximately 30% of healthy individuals, serving as a reservoir for infection under conducive conditions.
Common Risk Factors:
- Skin trauma (cuts, abrasions, surgical wounds)
- Immunocompromised status (HIV, cancer, diabetes)
- Close-contact environments (athletes, military personnel)
- Poor hygiene or skin barrier disruption
- Presence of indwelling devices or prosthetics
- Recent antibiotic use or hospitalization
Clinical Manifestations of Staphylococcus Skin Infections
The clinical presentation of staphylococcal SSSIs varies with the depth, location, and severity of the infection.
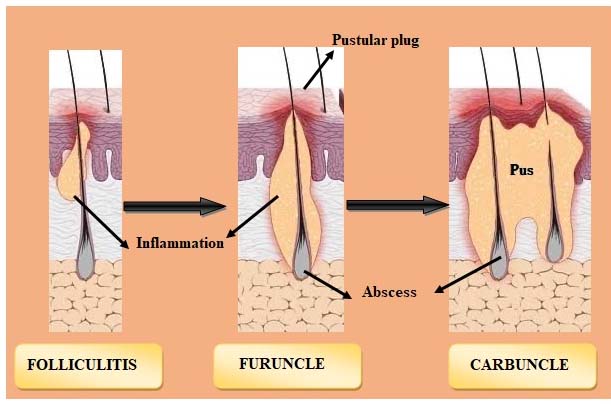
Superficial and Localized Forms:
- Folliculitis: Inflammation of hair follicles, presenting as small red pustules
- Furuncles (Boils): Deep folliculitis with painful, pus-filled nodules
- Carbuncles: Coalescence of multiple furuncles, often with systemic symptoms
Deeper or Severe Presentations:
- Cellulitis: Diffuse skin inflammation with redness, warmth, edema, and pain
- Abscesses: Localized collections of pus within the dermis or deeper layers
- Impetigo: Contagious blistering infection, more common in children
- Surgical Site Infections (SSI): Postoperative wound infections, often with drainage
- Necrotizing fasciitis: Rapidly spreading, life-threatening infection of fascia
Methicillin-Resistant Staphylococcus aureus (MRSA): A Clinical Challenge
MRSA represents a critical concern in both community-acquired and hospital-acquired infections. It resists beta-lactam antibiotics, making treatment choices more complex.
Risk Factors for MRSA SSSI:
- Prior colonization or infection with MRSA
- Recent hospitalization or surgery
- Chronic wounds or ulcers
- Contact sports or incarceration
- Living in crowded conditions
MRSA infections tend to be more aggressive, with increased risk of abscess formation and treatment failure if not properly addressed.
Diagnostic Workup of Staphylococcal SSSIs
Timely diagnosis facilitates targeted therapy and helps prevent progression or systemic spread.
Diagnostic Steps:
- Clinical evaluation: Visual and tactile assessment of lesion morphology and severity
- Specimen collection: Pus or tissue cultures from abscesses or surgical wounds
- Gram stain and culture: Reveal gram-positive cocci in clusters
- Blood cultures: Recommended if systemic symptoms (fever, hypotension) are present
- PCR for MRSA detection: Provides rapid identification of resistant strains
Recommended Treatment Strategies for Staphylococcus SSSI
Effective management of staphylococcal infections depends on the infection type, presence of abscess, patient comorbidities, and antimicrobial susceptibility.
Empiric Therapy Guidelines:
| Infection Type | Recommended Antibiotics |
|---|---|
| Mild to moderate MSSA | Cephalexin, dicloxacillin, or clindamycin |
| Suspected or confirmed MRSA | TMP-SMX, doxycycline, clindamycin, or linezolid |
| Severe or deep infections | IV vancomycin, daptomycin, or ceftaroline |
| Recurrent MRSA | Consider decolonization (mupirocin + chlorhexidine wash) |
Surgical Interventions:
- Incision and drainage (I&D) for abscesses is often the primary treatment.
- Debridement may be required for necrotizing infections or infected hardware.
- Wound care with antimicrobial dressings improves healing and reduces biofilm formation.
Complications of Untreated or Inadequately Managed Infections
Delayed or inappropriate therapy can result in severe outcomes:
- Bacteremia and sepsis
- Infective endocarditis
- Osteomyelitis
- Septic arthritis
- Chronic wounds or ulceration
- Recurrence or treatment resistance
Early identification and thorough management significantly reduce morbidity and healthcare burden.
Infection Prevention and MRSA Control Strategies
Preventing staphylococcal transmission, particularly MRSA, is critical in both community and healthcare settings.
Key Measures:
- Hand hygiene and personal hygiene reinforcement
- Avoid sharing personal items (razors, towels)
- Wound coverage and appropriate dressing
- Decolonization protocols for recurrent carriers
- Contact precautions in hospitals for MRSA-positive patients
Future Outlook: Resistance Patterns and Emerging Therapies
With the rise of multidrug-resistant Staphylococcus aureus strains, novel therapeutic agents and vaccines are under investigation. Promising avenues include:
- Lipoglycopeptides (dalbavancin, oritavancin)
- Anti-virulence strategies targeting toxins and adhesion
- Phage therapy in chronic or biofilm-associated infections
- Enhanced rapid diagnostics to guide real-time therapy
Skin and skin structure infections due to Staphylococcus aureus remain a predominant cause of morbidity across all healthcare settings. Prompt recognition, culture-based diagnosis, appropriate antibiotic use, and surgical management are cornerstones of care. A comprehensive, multidisciplinary strategy ensures optimal outcomes, particularly in the era of antimicrobial resistance.