Serratia, particularly Serratia marcescens, is a gram-negative, facultative anaerobic bacillus that is commonly associated with nosocomial infections. Though more frequently linked with urinary and respiratory tract infections, Serratia is a notable pathogen in skin and skin structure infections (SSSIs), especially in immunocompromised patients or those with indwelling devices. Its ability to produce biofilms and exhibit multidrug resistance complicates treatment and increases clinical burden.
Epidemiology and Risk Factors for Serratia SSSI
Serratia marcescens is found in various environmental reservoirs, including water, soil, and hospital surfaces. It typically colonizes compromised skin or mucosa, leading to infection under favorable conditions.
At-Risk Populations:
- Burn victims and surgical wound patients
- Immunosuppressed individuals (transplant recipients, chemotherapy patients)
- Neonates in intensive care units
- Patients with indwelling catheters or chronic ulcers
- Diabetics with peripheral vascular disease
Risk Factors:
- Broad-spectrum antibiotic use
- Prolonged hospitalization
- Poor wound hygiene or dressing techniques
- Moisture-associated skin damage
- Contaminated disinfectants or hospital instruments
Microbiology and Virulence Mechanisms
Serratia marcescens is distinguished by its ability to produce a characteristic red pigment, prodigiosin. It possesses several features that enhance its pathogenicity in SSSI cases:
- Biofilm formation: Protects against immune responses and antibiotics
- Hemolysins and proteases: Cause cellular destruction and tissue damage
- AmpC β-lactamase production: Confers resistance to multiple beta-lactam antibiotics
- Adhesion factors: Facilitate colonization of epithelial and subcutaneous tissues
Clinical Manifestations of Serratia Skin Infections
Serratia can present in various forms, often mimicking other gram-negative or mixed pathogen infections. Prompt identification is key to effective management.
Common Presentations:
- Cellulitis: Rapidly spreading erythema, warmth, swelling, and pain
- Abscesses: Fluctuant, pus-filled nodules with surrounding inflammation
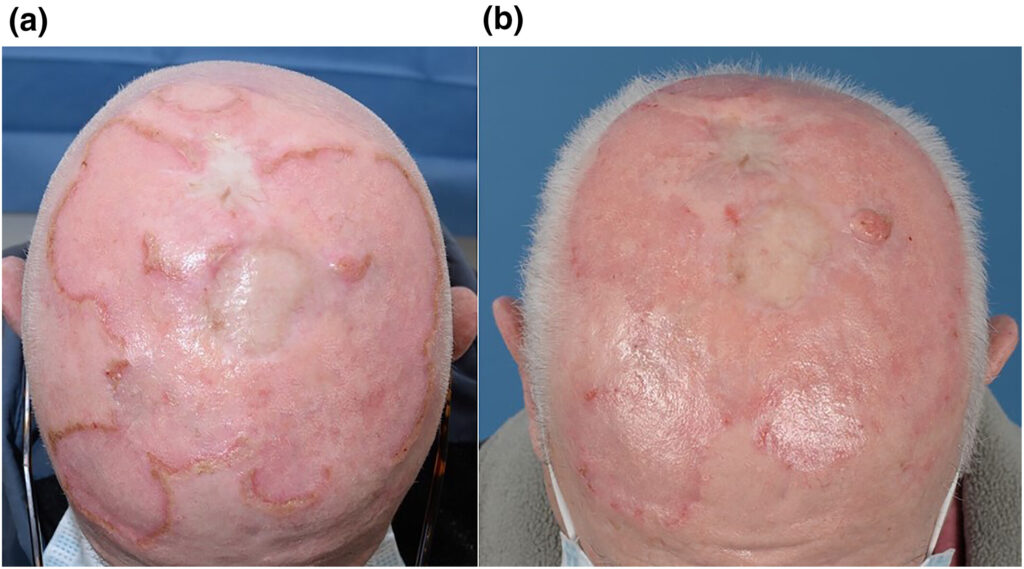
- Wound infections: Serosanguinous or purulent discharge, delayed healing, local necrosis
- Surgical site infections: Particularly in post-abdominal or orthopedic procedures
- Burn wound colonization/infection: Characterized by biofilm presence and delayed epithelialization
Diagnostic Approach for Serratia SSSI
Accurate and early identification is critical to guide treatment, given the potential for multidrug resistance and deep tissue involvement.
Recommended Diagnostic Steps:
- Clinical assessment: Evaluate lesion characteristics, systemic signs, and patient risk profile
- Specimen collection: Deep tissue biopsy or aspirated pus preferred over superficial swabs
- Gram stain and culture: Gram-negative bacilli with red-pigmented colonies (in some cases)
- Antibiotic sensitivity testing: Crucial to identify resistance, especially to beta-lactams and aminoglycosides
- Blood cultures: In systemic cases or immunocompromised hosts
Antibiotic Management of Serratia Skin Infections
Antimicrobial therapy should be initiated empirically in serious infections and refined based on sensitivity testing. Serratia marcescens is intrinsically resistant to ampicillin, first-generation cephalosporins, and macrolides.
Empirical and Targeted Antibiotics:
| Infection Type | Preferred Agents |
|---|---|
| Localized mild infection | Fluoroquinolones (e.g., ciprofloxacin), TMP-SMX (if susceptible) |
| Moderate to severe SSSI | Cefepime, meropenem, or piperacillin-tazobactam |
| MDR strains | Carbapenems (e.g., meropenem), tigecycline, or combination therapy with aminoglycosides |
| Resistant to carbapenems | Consider polymyxins (colistin) or newer agents like cefiderocol (if available) |
Duration of Therapy:
10–14 days, extendable for osteomyelitis or immunocompromised patients.
Surgical and Wound Care Interventions
Treatment of Serratia SSSIs is most effective when antibiotics are combined with thorough wound care and surgical management where necessary.
Surgical Measures:
- Incision and drainage (I&D): Essential for abscesses and deep collections
- Debridement: Removal of necrotic tissue to promote healing
- Skin grafting: For severe tissue loss, especially in burn wounds
Wound Care Principles:
- Use of antimicrobial dressings (e.g., silver or honey-based)
- Maintenance of moist wound healing environment
- Regular assessment and dressing changes
- NPWT (Negative Pressure Wound Therapy) in large or complex wounds
Complications and Clinical Concerns
Untreated or poorly managed Serratia infections can progress and cause:
- Bacteremia or sepsis
- Wound necrosis and extension into muscle layers
- Osteomyelitis in chronic wounds or diabetics
- Graft or implant infections
- Prolonged hospitalization and increased morbidity
Infection Control and Prevention in Healthcare Settings
Serratia has been implicated in numerous outbreaks due to its ability to survive in disinfectants and water-based solutions.
Prevention Strategies:
- Rigorous hand hygiene compliance
- Proper sterilization of surgical instruments and respiratory equipment
- Environmental decontamination of hospital surfaces
- Avoidance of shared personal care items in multi-bed wards
- Antimicrobial stewardship programs to reduce resistance pressure
Skin and skin structure infections caused by Serratia marcescens demand early recognition, microbiological confirmation, and appropriately guided antimicrobial therapy. Given its resistance patterns and the potential for deep-tissue complications, a multidisciplinary approach that includes infectious disease specialists, surgeons, and wound care professionals yields the best outcomes. Vigilant infection control practices are vital to prevent nosocomial spread and reinfection.