Pseudomonas aeruginosa is a gram-negative, opportunistic pathogen known for its role in healthcare-associated skin and skin structure infections (SSSIs). It poses a significant clinical challenge due to its intrinsic resistance mechanisms and its ability to thrive in moist, damaged, or necrotic tissue environments. These infections are especially prevalent among immunocompromised patients, individuals with burns, and those with chronic wounds.
Epidemiology and Risk Factors for P. aeruginosa SSSI
Common Patient Populations:
- Burn patients with extensive tissue damage
- Diabetic individuals with foot ulcers
- Post-operative patients with surgical site infections
- Immunocompromised hosts, including those with cancer or on immunosuppressive therapy
- Patients with indwelling devices or prolonged antibiotic exposure
Predisposing Factors:
- Moist environments (e.g., macerated skin)
- Breaches in skin integrity
- Frequent hospitalizations
- Poor glycemic control
- Presence of biofilms
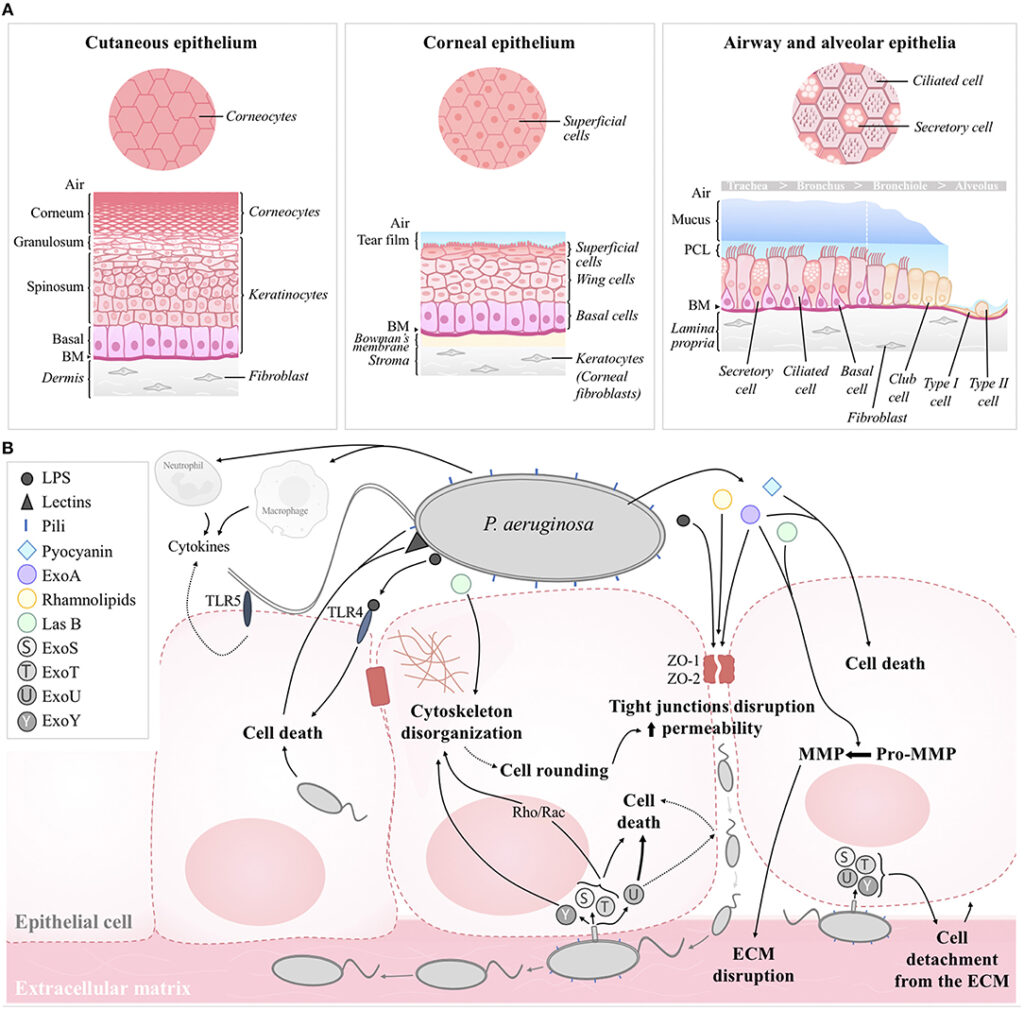
Pathophysiology and Virulence Mechanisms
P. aeruginosa utilizes an array of virulence factors that promote tissue invasion, immune evasion, and resistance to treatment:
- Exotoxin A: Inhibits host protein synthesis
- Elastase and proteases: Degrade extracellular matrix and immune proteins
- Pyocyanin: Generates reactive oxygen species, impairing healing
- Biofilm formation: Enhances survival in hostile environments and protects from antibiotics
- Efflux pumps and β-lactamases: Contribute to broad-spectrum antibiotic resistance
Clinical Presentations of Pseudomonas Skin Infections
Common Manifestations:
- Folliculitis: Often associated with contaminated hot tubs (hot tub rash)
- Ecthyma gangrenosum: Rapidly progressive necrotic lesion typically seen in neutropenic patients
- Cellulitis and abscesses: Painful, erythematous, and frequently purulent
- Wound infection: Foul-smelling, greenish exudate often visible in burn or surgical sites
- Chronic ulcers: Delayed healing due to persistent colonization and tissue damage
Diagnostic Approach to Skin and Skin Structure Infections by P. aeruginosa
Diagnostic Workflow:
- Clinical inspection: Note green-blue exudate, necrosis, or signs of systemic involvement
- Microbiological culture: Deep tissue swabs, wound aspirates, or biopsies should be obtained
- Gram staining: Presence of gram-negative rods supports initial suspicion
- Antibiotic sensitivity testing: Critical due to high prevalence of MDR and XDR strains
- Advanced imaging (CT/MRI): Consider if osteomyelitis or deep tissue involvement is suspected
Effective Antimicrobial Therapy for Pseudomonas SSSI
Given the bacterium’s resistance profile, treatment must be guided by susceptibility results. However, empirical therapy should be broad enough to cover potential resistance.
| Infection Severity | Recommended Antibiotics |
|---|---|
| Mild/moderate localized | Ciprofloxacin, levofloxacin (if susceptible) |
| Moderate/severe infections | Piperacillin-tazobactam, cefepime, ceftazidime, or meropenem |
| MDR/XDR strains | Colistin, ceftolozane-tazobactam, cefiderocol |
| Combination therapy | Often used in critically ill patients; e.g., beta-lactam + aminoglycoside |
Duration of therapy:
Typically 10–14 days, extendable for chronic or necrotic wounds or deeper involvement.
Surgical and Supportive Management
Pharmacological therapy alone is insufficient in most cases. A multimodal approach including surgical care ensures optimal recovery.
Surgical Interventions:
- Aggressive debridement: To eliminate necrotic tissue and reduce bacterial load
- Drainage of abscesses: Prevents systemic spread
- Skin grafting: May be needed in severe tissue loss or burn cases
Wound Care Protocols:
- Use of silver or iodine-based dressings
- Negative pressure wound therapy (NPWT)
- Regular dressing changes under sterile conditions
- Topical antimicrobials for superficial colonization
Complications and Long-Term Sequelae
If not managed promptly, P. aeruginosa infections can lead to:
- Sepsis or bacteremia
- Extensive tissue necrosis
- Osteomyelitis
- Amputation in diabetic foot infections
- Hospital-acquired pneumonia from wound colonization
- Delayed wound healing due to persistent colonization
Infection Control and Prevention Strategies
Hospital Measures:
- Strict hand hygiene and contact precautions
- Environmental decontamination
- Isolation of infected patients
- Antimicrobial stewardship to reduce selective pressure
Patient-Centered Approaches:
- Glycemic control in diabetic patients
- Regular foot inspection and wound monitoring
- Proper wound dressing and hygiene
- Avoidance of hot tubs or swimming pools with open wounds
Skin and skin structure infections caused by Pseudomonas aeruginosa require immediate and precise intervention due to their aggressive nature and resistance patterns. A comprehensive approach combining clinical assessment, microbiologic diagnosis, targeted antibiotics, and effective wound management is crucial. Multidisciplinary coordination among infectious disease specialists, surgeons, and wound care teams enhances patient outcomes and minimizes complications.