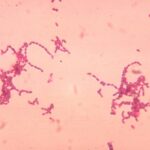
Proteus species, particularly Proteus mirabilis and Proteus vulgaris, are facultatively anaerobic gram-negative bacilli belonging to the Enterobacteriaceae family. While commonly residing in the gastrointestinal tract, these organisms can become opportunistic pathogens in skin and soft tissue infections (SSSIs), particularly when normal barriers are compromised.
Their motility (via peritrichous flagella) and urease activity contribute to their pathogenicity in both urinary and cutaneous infections. In wound environments, Proteus is associated with malodorous, necrotic infections and often forms part of polymicrobial biofilms.

Pathophysiology of Proteus-Related Cutaneous Infections
Upon breach of the skin barrier—typically through trauma, surgical intervention, or ulceration—Proteus species colonize and proliferate in nutrient-rich, poorly perfused tissues. Key pathogenic mechanisms include:
- Urease production: Alters local pH, impairing immune response.
- Biofilm formation: Enhances antibiotic resistance and persistence.
- Tissue-degrading enzymes: Promote necrosis and abscess development.
These features render Proteus infections challenging to treat, especially in chronic wounds or immunocompromised individuals.
Common Risk Factors and Predisposing Conditions
| Risk Factor | Contribution to Infection |
|---|---|
| Chronic pressure ulcers | Provide anaerobic, nutrient-rich environments |
| Diabetes mellitus | Compromised immune function and delayed healing |
| Surgical wounds | Disruption of sterile barriers |
| Urinary or fecal incontinence | Local contamination and perineal skin maceration |
| Immunosuppression | Increased susceptibility to opportunistic pathogens |
Clinical Presentation of Proteus Skin and Soft Tissue Infections
Skin and skin structure Proteus infections can vary in presentation depending on the depth and severity of involvement. Key clinical manifestations include:
- Malodorous, purulent discharge from wounds
- Localized cellulitis with redness, warmth, and swelling
- Necrotic tissue or slough in chronic ulcers
- Systemic symptoms such as fever and leukocytosis in severe cases
- Non-healing surgical wounds despite standard care
In patients with polymicrobial infections, Proteus often acts synergistically with other facultative or anaerobic organisms.
Diagnostic Evaluation of Proteus Cutaneous Infections
Clinical Examination
- Assessment of wound edges, presence of odor, and extent of necrosis
- Evaluation for signs of systemic spread (fever, tachycardia, hypotension)
Microbiological Analysis
- Wound swab or tissue culture: Confirmatory growth of Proteus mirabilis or Proteus vulgaris
- Gram stain: Gram-negative rods, often in conjunction with other bacteria
- Antibiotic susceptibility testing: Essential due to increasing resistance patterns
Imaging Studies
- Ultrasound or CT scan: To detect underlying abscesses or foreign bodies
- MRI: Preferred for evaluating involvement of deep fascia or bone
Recommended Antimicrobial Therapy for Proteus Infections
Empirical treatment should be guided by the site, severity, and comorbidities, and subsequently refined by culture results.
| Infection Severity | Preferred Antibiotic Regimens |
|---|---|
| Mild | Amoxicillin-clavulanate, trimethoprim-sulfamethoxazole (TMP-SMX) |
| Moderate to severe | Piperacillin-tazobactam, cefepime, meropenem |
| Resistant strains | Consider carbapenems or combination therapy guided by antibiogram |
| Penicillin allergy | Aztreonam + metronidazole, or ciprofloxacin + clindamycin |
Duration typically ranges from 7 to 21 days, depending on clinical response and wound healing.
Surgical and Supportive Management
Surgical Intervention
- Debridement: Removal of necrotic tissue to prevent spread
- Drainage of abscesses: Ensures reduction in bacterial load
- Wound closure strategies: May include secondary intention or grafting in chronic cases
Supportive Measures
- Wound care: Regular dressing changes, moisture balance, and infection monitoring
- Glycemic control: Critical for diabetic wound healing
- Nutritional support: Improves tissue regeneration and immune defense
Complications of Untreated Proteus Skin Infections
- Deep tissue necrosis and progression to fasciitis
- Chronic wound colonization and delayed closure
- Septicemia in cases of uncontrolled infection
- Antibiotic-resistant strains leading to therapeutic failure
Early intervention minimizes the likelihood of these complications and improves prognosis significantly.
Preventive Strategies and Risk Reduction
Clinical Guidelines
- Preoperative skin cleansing and prophylaxis in high-risk surgeries
- Sterile technique during dressing changes and wound interventions
- Early management of chronic ulcers and incontinence-associated dermatitis
Patient Education
- Hygiene practices: Essential for patients with chronic wounds or incontinence
- Wound monitoring: Prompt identification of changes in odor, drainage, or pain
- Compliance with antibiotics and follow-up appointments
Skin and skin structure infections caused by Proteus species represent a significant challenge in clinical practice, particularly in high-risk and immunocompromised patients. Successful management requires a multifaceted approach combining timely diagnosis, appropriate antibiotic therapy, surgical intervention, and comprehensive wound care. By implementing evidence-based strategies, clinicians can effectively control infection, promote healing, and prevent recurrence.