Peptococcus species are gram-positive, obligate anaerobic cocci that form part of the normal human flora, particularly in the gastrointestinal and genitourinary tracts. Although generally considered non-pathogenic, under certain conditions such as immunosuppression, trauma, or surgical intervention, Peptococcus can become opportunistic, leading to serious skin and skin structure infections (SSSIs).

Pathophysiology of Peptococcus in Soft Tissue Infections
Peptococcus contributes to infection primarily in mixed anaerobic polymicrobial environments. These organisms thrive in necrotic tissue with reduced oxygen supply, often in conjunction with Bacteroides, Prevotella, or facultative aerobes like Staphylococcus aureus. The anaerobic environment facilitates:
- Tissue necrosis and abscess formation
- Suppressed local immune response
- Enhanced toxin and enzyme release by co-infecting bacteria
The infection frequently progresses insidiously and can become chronic if not addressed promptly.
Risk Factors for Developing Peptococcus Skin and Soft Tissue Infections
| Risk Factor | Description |
|---|---|
| Diabetic foot ulcers | Reduced perfusion and impaired healing |
| Deep bite wounds or trauma | Entry of anaerobes into subcutaneous tissues |
| Post-surgical infections | Especially in perineal or abdominal surgeries |
| Immunocompromised status | Cancer, HIV, steroid use |
| Poor wound hygiene | Promotes anaerobic colonization |
| Prolonged antibiotic use | Disruption of normal flora |
Clinical Features of Peptococcus-Associated SSSIs
The presentation of Peptococcus infections varies depending on depth and anatomical site. Common manifestations include:
Abscesses
Localized collections of pus with fluctuance, erythema, and tenderness. Anaerobic abscesses tend to have foul-smelling discharge.
Cellulitis with Necrosis
Infection spreads across tissue planes, often with crepitus, skin discoloration, and systemic toxicity in severe cases.
Post-operative Wound Infections
Delayed healing, purulent drainage, and local swelling at surgical sites, especially in abdominal or pelvic procedures.
Diagnostic Workup for Skin and Skin Structure Peptococcus Infections
Clinical Examination
Initial diagnosis is based on localized skin findings and systemic signs such as fever, leukocytosis, or hypotension.
Laboratory and Imaging Investigations
- Anaerobic culture from wound swabs or aspirated pus
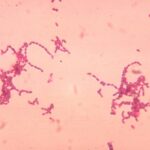
- Gram staining: Shows gram-positive cocci in clusters
- CBC and CRP/ESR for inflammation monitoring
- Imaging (CT or MRI) to detect gas formation or abscess cavities
Antimicrobial Susceptibility and Resistance Profile
Peptococcus species are typically sensitive to:
- Penicillin G
- Clindamycin
- Metronidazole
- Imipenem
However, resistance to macrolides and tetracyclines has been observed. Empiric therapy should be adjusted based on susceptibility patterns, especially in polymicrobial settings.
Treatment of Peptococcus Skin and Soft Tissue Infections
Empiric Antimicrobial Therapy
| Infection Type | Recommended Agents |
|---|---|
| Mild/moderate infections | Amoxicillin-clavulanate, clindamycin, or metronidazole |
| Severe or deep infections | Piperacillin-tazobactam, imipenem, or meropenem |
Duration typically ranges from 10 to 14 days, adjusted based on response and infection resolution.
Surgical Management
- Incision and Drainage (I&D) for abscesses
- Debridement of necrotic or infected tissue
- Vacuum-Assisted Closure (VAC) therapy for chronic wounds
Complications Associated with Peptococcus Skin Infections
Without prompt intervention, Peptococcus infections may result in:
- Chronic draining sinuses
- Fistula formation
- Necrotizing fasciitis
- Osteomyelitis in adjacent bones
- Bacteremia and sepsis
Patients with diabetes or vascular disease are at higher risk for limb-threatening complications.
Preventive Strategies and Infection Control
Clinical Practices
- Maintain surgical asepsis
- Use prophylactic antibiotics where indicated
- Monitor high-risk surgical wounds closely
Community and Outpatient Settings
- Educate on proper wound care and hygiene
- Encourage early consultation for infected wounds
- Optimize management of comorbid conditions like diabetes
Skin and skin structure infections caused by Peptococcus demand timely recognition and multidisciplinary management. These anaerobic pathogens, though often part of the body’s normal flora, can lead to severe complications when introduced into compromised tissue environments. Comprehensive treatment—combining targeted antibiotic therapy, surgical intervention, and proper wound care—ensures favorable outcomes and prevents chronic or systemic spread.