Acinetobacter species, particularly Acinetobacter baumannii, are gram-negative, opportunistic pathogens implicated in a range of healthcare-associated infections. Among these, skin and skin structure infections (SSTIs) pose significant challenges due to the organism’s ability to survive in hospital environments and its high resistance to antibiotics.
SSTIs caused by Acinetobacter typically affect immunocompromised patients, trauma victims, burn patients, and those with open wounds. These infections range from superficial cellulitis to deep-seated necrotizing fasciitis.
Epidemiology and Risk Factors
Prevalence:
Acinetobacter infections have risen sharply, especially in intensive care units (ICUs) and among patients undergoing surgical or orthopedic procedures.
Risk Factors Include:
- Prolonged hospitalization
- Use of invasive devices (e.g., catheters, central lines)
- Open wounds or surgical incisions
- Burns and traumatic injuries
- Immunosuppression or diabetes mellitus
- Previous antibiotic exposure
Pathogenesis of Acinetobacter in SSTIs
Acinetobacter can colonize intact skin and mucosal surfaces. Upon disruption of the skin barrier, it gains entry into subcutaneous tissues, leading to infection. The pathogen’s ability to form biofilms enhances its survival and resistance in wound environments.
Virulence Mechanisms:
- Outer membrane proteins facilitating adhesion
- Enzyme production (lipases, proteases)
- Biofilm formation on skin and wound surfaces
- Resistance to desiccation and disinfectants
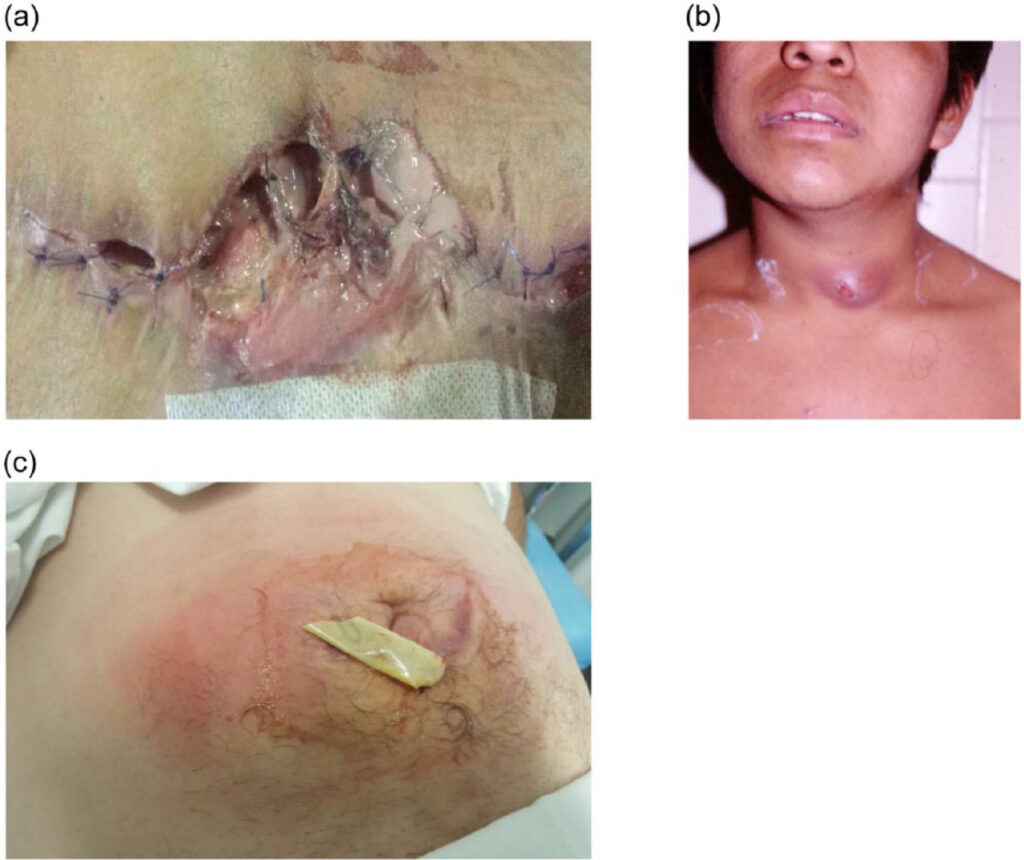
Clinical Manifestations
Skin and skin structure Acinetobacter infections may present in multiple forms, depending on depth, patient immunity, and presence of foreign material.
Common Presentations:
- Cellulitis: Diffuse erythema, warmth, and swelling
- Wound infection: Purulent discharge, delayed healing
- Abscess formation: Localized collections requiring drainage
- Necrotizing fasciitis: Rapidly progressing infection with systemic toxicity
- Burn wound colonization: High risk of systemic spread
Diagnostic Approach
Clinical Evaluation:
- Inspection of wound, surgical site, or skin lesion
- Assessment of systemic symptoms (fever, hypotension, leukocytosis)
Microbiological Confirmation:
- Specimen Collection: Tissue biopsy or deep wound swab
- Culture and Sensitivity Testing: Determines antibiotic susceptibility
- Molecular Diagnostics: PCR assays for resistance genes (e.g., OXA, NDM)
Antimicrobial Resistance Profile
Acinetobacter species, especially A. baumannii, exhibit resistance to multiple drug classes, complicating treatment.
Common Resistance Patterns:
| Antibiotic Class | Resistance Mechanism |
|---|---|
| Beta-lactams | Beta-lactamase enzymes (OXA-type carbapenemases) |
| Aminoglycosides | Enzymatic modification, 16S rRNA methylation |
| Fluoroquinolones | Mutations in DNA gyrase/topoisomerase |
| Carbapenems | OXA-type carbapenemases, efflux pumps |
Multidrug-Resistant (MDR) strains are defined as those resistant to at least three different antimicrobial classes.
Therapeutic Strategies
Effective treatment requires a combination of surgical intervention and targeted antimicrobial therapy based on culture results.
Empirical Therapy
Initiated in severe infections before culture results are available, especially in ICU or trauma settings.
Options May Include:
- Colistin (polymyxin E)
- Tigecycline
- Sulbactam-containing combinations
- Minocycline
- Cefiderocol (in resistant cases)
Targeted Therapy
Refined according to sensitivity profile. Monotherapy or combination regimens may be used depending on severity and resistance.
| Agent | Role in Therapy |
|---|---|
| Colistin | Reserved for MDR pathogens, nephrotoxic |
| Tigecycline | Effective in soft tissue, not bloodstream |
| Sulbactam | Has intrinsic activity against Acinetobacter |
| Cefiderocol | New siderophore cephalosporin for XDR cases |
Surgical Management
- Incision and drainage of abscesses
- Debridement of necrotic tissue
- Negative pressure wound therapy (NPWT) in complex wounds
Infection Control and Prevention
Preventing skin and soft tissue Acinetobacter infections in healthcare settings is essential.
Key Measures:
- Strict hand hygiene protocols
- Contact precautions for infected or colonized patients
- Environmental decontamination
- Antimicrobial stewardship programs to minimize resistance
- Surveillance cultures in high-risk units
Prognosis and Outcomes
The prognosis depends on early diagnosis, appropriate antibiotic use, and timely surgical intervention. MDR infections are associated with longer hospital stays, increased costs, and higher mortality rates.
Factors Associated with Poor Outcome:
- Delay in effective therapy
- Extensive tissue involvement
- Septic complications
- Infections with extensively drug-resistant (XDR) strains
Acinetobacter-related skin and skin structure infections represent a significant clinical challenge due to the organism’s resilience and antibiotic resistance. Accurate diagnosis, early targeted antimicrobial therapy, and appropriate surgical management are pivotal in improving outcomes. Preventive strategies remain the cornerstone in controlling hospital-associated spread, especially in vulnerable populations.