Patients who develop opioid tolerance often experience diminished analgesic effects despite increasing dosages, leading to refractory severe pain. This condition presents one of the most challenging scenarios in pain medicine, requiring a nuanced approach that balances effective analgesia with safety and risk mitigation.
Mechanisms Behind Opioid Tolerance
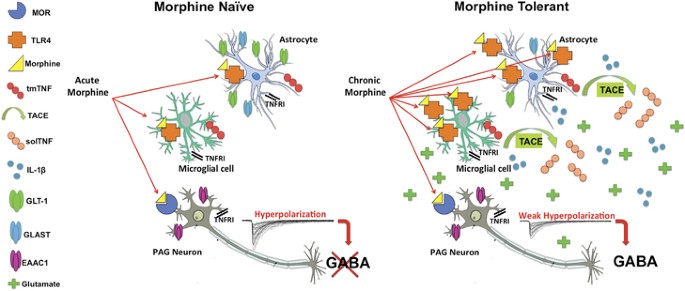
Opioid tolerance is a pharmacological phenomenon characterized by reduced responsiveness to opioid agonists over time. Key contributing mechanisms include:
- Receptor desensitization: μ-opioid receptor downregulation and altered intracellular signaling.
- Neuroplasticity: Sensitization of pain pathways and upregulation of pronociceptive systems.
- Opioid-induced hyperalgesia: Paradoxical increase in pain sensitivity despite opioid use.
Clinical Identification of Opioid Tolerance
Diagnostic Indicators
- Escalating opioid doses with inadequate pain control
- Reduced duration of analgesic relief
- Increasing side effects without proportional benefit
- Evidence of opioid-induced hyperalgesia (OIH)
Pain Assessment Tools
- Numeric Rating Scale (NRS)
- Visual Analog Scale (VAS)
- Brief Pain Inventory (BPI)
- PainDETECT Questionnaire for neuropathic components
Multimodal Management Strategies
1. Opioid Rotation and Cross-Tapering
Switching to an alternative opioid with incomplete cross-tolerance may restore analgesic efficacy. This process includes:
- Calculating equianalgesic doses
- Applying a 25–50% dose reduction for cross-tolerance
- Monitoring for breakthrough pain and adverse effects
Common Rotational Examples:
- Morphine → Hydromorphone
- Oxycodone → Methadone
- Fentanyl → Buprenorphine
2. Adjuvant Analgesics
Adjunct medications target specific pain mechanisms and reduce opioid reliance:
| Class | Examples | Indications |
|---|---|---|
| Anticonvulsants | Gabapentin, Pregabalin | Neuropathic pain, fibromyalgia |
| Antidepressants | Duloxetine, Amitriptyline | Neuropathic pain, mood modulation |
| NMDA Receptor Antagonists | Ketamine, Methadone | Opioid-induced hyperalgesia, tolerance |
| Corticosteroids | Dexamethasone | Inflammatory or neoplastic pain |
3. Interventional Pain Procedures
When pharmacotherapy is insufficient, targeted interventions are considered.
- Spinal cord stimulation (SCS): Especially effective for failed back surgery syndrome and CRPS.
- Intrathecal pump therapy: Allows direct spinal administration of opioids or non-opioids at lower doses.
- Peripheral nerve blocks: Immediate relief for localized somatic pain.
4. Non-Pharmacological Therapies
Cognitive and Behavioral Approaches
- Cognitive Behavioral Therapy (CBT)
- Mindfulness-Based Stress Reduction (MBSR)
- Acceptance and Commitment Therapy (ACT)
These approaches enhance coping mechanisms, reduce pain-related distress, and limit opioid reliance.
Physical Rehabilitation
- Structured physical therapy programs
- Aquatic therapy for low-impact conditioning
- Functional restoration programs to rebuild strength and endurance
Advanced Therapies: Ketamine and Buprenorphine
Ketamine Infusion
- NMDA receptor antagonist
- Used in opioid-refractory pain, especially when hyperalgesia is present
- Low-dose, sub-anesthetic infusions reduce central sensitization
Buprenorphine Transition
- Partial μ-opioid agonist with high receptor affinity
- Effective for patients requiring opioid weaning or exhibiting signs of misuse
- Can be administered via patch, sublingual tablet, or injection
Risks and Considerations in Management
Opioid Stewardship
- Utilize Prescription Drug Monitoring Programs (PDMPs)
- Establish clear treatment goals and reassessment intervals
- Consider urine drug screening to ensure compliance
Preventing Opioid Misuse and Diversion
- Employ risk assessment tools such as the ORT (Opioid Risk Tool)
- Use of abuse-deterrent opioid formulations
- Close coordination with addiction specialists when needed
Long-Term Outlook and Goals
Management of severe pain in opioid-tolerant patients demands a personalized, interdisciplinary plan. The goal is not merely pain relief but functional restoration and enhanced quality of life. Achieving these outcomes requires coordinated input from pain specialists, primary care providers, mental health professionals, and rehabilitation teams.
Severe pain with opioid tolerance is a complex clinical condition requiring strategic, multifaceted intervention. By combining evidence-based pharmacologic approaches, advanced procedural techniques, and non-pharmacological therapies, we can reduce suffering and improve outcomes even in opioid-refractory cases. Emphasis on opioid stewardship, individualized care, and continuous reassessment remains essential to success.