Severe insomnia is a complex and persistent sleep disorder characterized by difficulty initiating or maintaining sleep, or by waking too early and being unable to return to sleep. It becomes clinically significant when it impairs daily functioning and persists for at least three nights per week for three months or longer. Unlike transient or short-term insomnia, severe insomnia often has multifactorial origins and requires a multidisciplinary treatment approach.

Types and Clinical Presentation of Insomnia
Classification of Insomnia Disorders
- Acute Insomnia – Short-term, often triggered by stress or environmental change
- Chronic Insomnia – Lasting three months or longer, often linked to comorbid medical or psychiatric conditions
- Primary Insomnia – Not caused by another health condition
- Secondary Insomnia – Caused by medications, medical conditions, or psychiatric disorders
Symptoms of Severe Insomnia
- Difficulty falling asleep (>30 minutes latency)
- Frequent awakenings during the night
- Waking up too early without being able to return to sleep
- Daytime fatigue, irritability, or difficulty concentrating
- Reduced occupational or social performance
- Sleep dissatisfaction despite adequate opportunity to sleep
Pathophysiology of Severe Insomnia
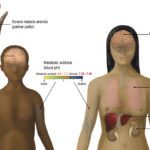
The underlying mechanisms of severe insomnia involve heightened arousal of the central nervous system, cognitive distortions around sleep, and dysregulation of circadian rhythms. Neuroimaging studies have shown increased metabolic activity in wake-promoting brain regions even during attempted sleep.
Common Causes and Risk Factors
Psychological and Behavioral Factors
- Generalized anxiety disorder
- Major depressive disorder
- Post-traumatic stress disorder
- Poor sleep habits and irregular schedules
- Learned sleep-preventing behaviors
Medical and Physiological Triggers
- Chronic pain conditions
- Hyperthyroidism
- Asthma or chronic obstructive pulmonary disease (COPD)
- Neurological disorders such as Parkinson’s or Alzheimer’s disease
Environmental and Lifestyle Contributors
- Excessive screen time before bed
- Stimulant use (caffeine, nicotine)
- Jet lag or shift work
- Noise or light pollution
Diagnostic Evaluation of Chronic Insomnia
Comprehensive Sleep History
A structured sleep interview should assess sleep patterns, latency, duration, disturbances, and daytime consequences. Sleep diaries and standardized questionnaires such as the Insomnia Severity Index (ISI) provide objective insights.
Polysomnography and Actigraphy
Polysomnography is reserved for differential diagnosis (e.g., sleep apnea, periodic limb movement disorder). Actigraphy helps assess sleep-wake cycles over days to weeks, especially in cases of circadian rhythm disorders.
Evidence-Based Treatment for Severe Insomnia
Cognitive Behavioral Therapy for Insomnia (CBT-I)
CBT-I remains the gold standard for chronic insomnia treatment. It targets maladaptive beliefs and behaviors that perpetuate sleep problems.
Core Components of CBT-I:
- Stimulus control therapy – Strengthens bed-sleep association
- Sleep restriction – Reduces time in bed to match actual sleep time
- Cognitive restructuring – Challenges irrational thoughts about sleep
- Relaxation training – Lowers pre-sleep arousal
- Sleep hygiene education – Optimizes environmental and behavioral factors
Pharmacological Management
Medications are used when non-pharmacological strategies are insufficient, ideally for short durations under clinical supervision.
Commonly Prescribed Agents:
- Benzodiazepine receptor agonists (e.g., zolpidem, eszopiclone)
- Melatonin receptor agonists (e.g., ramelteon)
- Sedating antidepressants (e.g., doxepin, trazodone)
- Dual orexin receptor antagonists (e.g., suvorexant, lemborexant)
Caution is advised due to tolerance, dependence, and next-day sedation risks.
Lifestyle Modifications and Sleep Hygiene
Adhering to disciplined bedtime routines and environmental optimizations can significantly enhance sleep quality.
Recommended Practices:
- Maintain a consistent sleep-wake schedule
- Avoid electronic screens 1–2 hours before bed
- Keep the bedroom dark, quiet, and cool
- Limit caffeine and alcohol, especially in the evening
- Use the bed exclusively for sleep and intimacy
Complications of Untreated Severe Insomnia
Chronic insomnia has wide-ranging consequences:
- Increased risk of hypertension, obesity, and type 2 diabetes
- Higher incidence of cardiovascular disease
- Elevated rates of depression and suicidal ideation
- Reduced immune function
- Impaired cognitive performance and memory consolidation
Addressing insomnia early is essential to avoid long-term health deterioration.
Managing Insomnia in Special Populations
Elderly Individuals
Age-related changes in sleep architecture (e.g., decreased slow-wave sleep) make older adults more susceptible. CBT-I is effective and preferred over pharmacotherapy due to heightened fall risk.
Pregnant Women
Insomnia is common due to hormonal shifts, physical discomfort, and anxiety. Non-drug therapies, such as mindfulness and CBT-I, are first-line.
Individuals with Comorbid Psychiatric Illness
Co-treatment of both insomnia and the psychiatric disorder yields better outcomes. Collaborative care involving psychiatry and sleep medicine is recommended.
Prognosis and Long-Term Outlook
With timely and targeted intervention, severe insomnia can be successfully managed. A significant percentage of individuals achieve sustained improvements in sleep with CBT-I. Lifelong adherence to good sleep hygiene and periodic reassessment is key to preventing relapse.
Severe insomnia is a serious yet treatable condition with far-reaching health implications. A structured approach combining behavioral therapy, lifestyle adjustments, and, when appropriate, short-term pharmacologic intervention offers the best outcomes. Personalized care based on patient history, comorbidities, and treatment response ensures optimal recovery of sleep health and daily functioning.