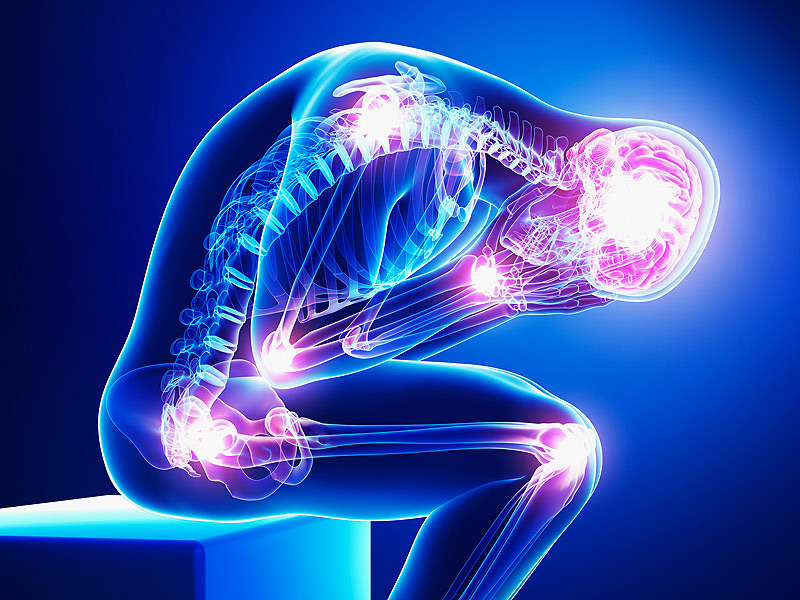
Severe chronic pain is defined as persistent or recurrent pain lasting longer than three months that significantly impairs physical function, emotional well-being, and overall quality of life. It often persists beyond the normal healing period and may arise without an identifiable ongoing cause. This condition affects millions globally, burdening healthcare systems and individuals alike with long-term disability and psychosocial stress.
Types of Severe Chronic Pain
Neuropathic Pain
Resulting from nerve damage or dysfunction, neuropathic pain includes conditions such as diabetic neuropathy, postherpetic neuralgia, and radiculopathy. Symptoms often involve burning, tingling, and electric shock-like sensations.
Nociceptive Pain
Originates from tissue injury or inflammation. It may be classified as:
- Somatic pain – localized to skin, muscles, or joints
- Visceral pain – arises from internal organs
Mixed Pain Syndromes
Examples include fibromyalgia and complex regional pain syndrome (CRPS), involving both nociceptive and neuropathic mechanisms.
Common Causes of Severe Chronic Pain
| Condition | Description |
|---|---|
| Fibromyalgia | Widespread musculoskeletal pain with fatigue and mood issues |
| Arthritis (Osteo & Rheumatoid) | Joint inflammation leading to stiffness and long-term pain |
| Spinal Disorders | Herniated discs, spinal stenosis, and degenerative diseases |
| Cancer Pain | Pain from tumors, metastases, or treatments |
| Post-surgical or Injury Pain | Persistent pain after trauma or surgery |
| Peripheral Neuropathy | Often due to diabetes, infections, or toxins |
Pathophysiology of Chronic Pain
Chronic pain involves changes in the central and peripheral nervous system:
Central sensitization enhances pain perception, even in the absence of ongoing injury. Neuroinflammation and maladaptive neuroplasticity contribute to the maintenance of chronic pain.
Symptoms of Severe Chronic Pain
- Persistent, intense pain (burning, throbbing, stabbing, or aching)
- Hypersensitivity to touch (allodynia) or amplified response to pain (hyperalgesia)
- Fatigue, poor sleep, and cognitive impairments (“brain fog”)
- Emotional symptoms: depression, anxiety, irritability
- Reduced mobility and social withdrawal
Diagnostic Approach to Severe Chronic Pain
Comprehensive Assessment
- Medical history and pain diaries
- Physical examination focusing on neurological signs
- Psychosocial evaluation for anxiety, depression, or PTSD
Diagnostic Tools
- Imaging (MRI, CT scans) to detect structural issues
- Nerve conduction studies and EMG for neuropathic pain
- Blood tests to rule out systemic causes (e.g., inflammation, vitamin deficiencies)
Medical Treatment Options for Chronic Pain
Pharmacologic Therapies
| Drug Class | Examples | Indications |
|---|---|---|
| NSAIDs | Ibuprofen, Naproxen | Inflammatory pain |
| Antidepressants | Amitriptyline, Duloxetine | Neuropathic pain, fibromyalgia |
| Anticonvulsants | Gabapentin, Pregabalin | Nerve pain |
| Opioids (last resort) | Morphine, Oxycodone | Severe, refractory pain |
| Topical Agents | Lidocaine, Capsaicin | Localized neuropathic pain |
Interventional Procedures
- Nerve blocks – temporary or diagnostic pain relief
- Epidural steroid injections – for spinal inflammation
- Radiofrequency ablation – destroys nerve fibers transmitting pain
- Spinal cord stimulators – modulate pain signals electronically
Non-Pharmacologic Management of Severe Chronic Pain
Physical Therapy
- Stretching, strengthening, and posture correction
- Restores mobility and reduces pain perception
Cognitive Behavioral Therapy (CBT)
- Alters pain-related thoughts and behaviors
- Proven to improve coping and emotional outcomes
Mindfulness and Relaxation Techniques
- Meditation, breathing exercises, and biofeedback
- Decrease pain intensity and improve mental health
Complementary Therapies
- Acupuncture
- Massage therapy
- Chiropractic manipulation
- Transcutaneous electrical nerve stimulation (TENS)
Lifestyle Strategies and Support Systems
Diet and Nutrition
- Anti-inflammatory diets rich in omega-3s and antioxidants
- Avoid processed foods, refined sugars, and trans fats
Sleep Hygiene
- Regular sleep schedule, dark and quiet environment
- Limit stimulants and screen time before bed
Social Support and Group Therapy
- Pain support groups reduce isolation
- Family education enhances home-based care
Chronic Pain in Special Populations
Older Adults
- Higher prevalence of osteoarthritis and spinal stenosis
- Increased risk of polypharmacy and drug side effects
Children and Adolescents
- May develop chronic pain from injuries, juvenile arthritis, or psychosocial stress
- Requires interdisciplinary pediatric pain management
Individuals with Disabilities
- Chronic pain worsens functional limitations
- Customized therapy plans needed for mobility-impaired individuals
Multidisciplinary Approach to Chronic Pain
Effective management requires coordination among:
- Primary care physicians
- Pain specialists
- Physical therapists
- Psychologists and psychiatrists
- Occupational therapists
- Nutritionists
Long-Term Outlook and Prognosis
The prognosis of severe chronic pain varies based on etiology, access to care, and adherence to treatment. While complete pain elimination is rare, significant improvements in functionality and quality of life are achievable with a structured, individualized care plan.
Severe chronic pain is a complex and multifactorial condition demanding a holistic, evidence-based approach. Early diagnosis, comprehensive assessment, and a multidisciplinary management strategy are vital for alleviating suffering and restoring quality of life. Empowering patients through education, consistent care, and support structures is essential for long-term success in chronic pain management.