Septic arthritis, also known as infectious arthritis, is a rapidly progressing joint infection caused primarily by bacterial pathogens. The condition involves invasion of the synovial membrane by microorganisms, leading to inflammation, cartilage destruction, and potential joint deformity. Timely diagnosis and intervention are vital to prevent permanent joint damage and systemic complications.

Etiology: Common Pathogens Causing Septic Arthritis
The causative organisms of septic arthritis vary by age group, immune status, and route of infection. The most frequently implicated pathogens include:
- Staphylococcus aureus (most common in all age groups)
- Streptococcus species
- Neisseria gonorrhoeae (in sexually active adults)
- Gram-negative bacilli (particularly in immunocompromised or elderly individuals)
- Kingella kingae (in children under 4 years)
- Mycobacterium tuberculosis and fungal pathogens in chronic or immunosuppressed patients
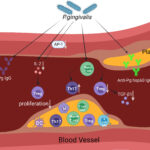
Pathogenesis of Septic Arthritis
Pathogens reach the joint via:
- Hematogenous spread (most common route)
- Direct inoculation (trauma, surgery, intra-articular injections)
- Contiguous spread from adjacent infected tissues
Once inside the joint, the bacteria trigger an inflammatory response involving neutrophil infiltration, release of proteolytic enzymes, and cytokine-mediated cartilage damage.
Clinical Presentation of Septic Arthritis
Septic arthritis typically presents with acute onset of symptoms involving a single joint (monoarthritis), although polyarticular involvement may occur, particularly in immunocompromised individuals.
Common symptoms include:
- Sudden, severe joint pain
- Joint swelling and erythema
- Warmth over the affected area
- Restricted range of motion
- Fever and chills
- Malaise or systemic signs of infection
The knee joint is most commonly affected, followed by the hip, shoulder, elbow, and wrist.
Diagnostic Evaluation of Septic Arthritis
Prompt and accurate diagnosis is essential. The following diagnostic measures should be undertaken:
Synovial Fluid Analysis (Gold Standard)
- Aspiration before antibiotics
- Appearance: Turbid or purulent
- WBC count: Typically >50,000 cells/µL with neutrophilic predominance
- Gram stain and culture: To identify causative organism
- Crystal analysis: To rule out crystal arthropathy
Blood Tests
- Elevated white blood cell count (WBC)
- C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR)
- Positive blood cultures (in up to 50% of cases)
Imaging Studies
- X-ray: May show joint space narrowing or bony erosions in chronic stages
- Ultrasound: Useful for detecting effusions
- MRI: Detailed evaluation of joint and adjacent structures, particularly in deep joints like the hip
Differential Diagnosis
It is critical to differentiate septic arthritis from other joint disorders such as:
- Gout or pseudogout
- Reactive arthritis
- Rheumatoid arthritis
- Hemarthrosis
- Osteomyelitis with adjacent joint involvement
Management and Treatment of Septic Arthritis
Empiric Antimicrobial Therapy
Initiation of empiric IV antibiotics is crucial and should be adjusted based on culture results.
Initial empiric choices include:
- Vancomycin (for MRSA coverage)
- Plus Ceftriaxone or Cefotaxime (for gram-negative coverage)
Duration:
- 2–4 weeks IV followed by oral therapy if appropriate
Joint Drainage
Effective drainage of purulent material is essential:
- Needle aspiration: Preferred in superficial joints
- Arthroscopic lavage: Minimally invasive and highly effective
- Open surgical drainage: For complex cases or failure of conservative measures
Supportive Measures
- Immobilization during the acute phase
- Gradual mobilization and physiotherapy after infection control
- Pain management with NSAIDs or acetaminophen
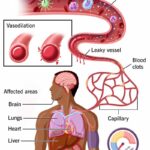
Complications of Untreated or Delayed Septic Arthritis
- Irreversible cartilage destruction
- Joint ankylosis or deformity
- Osteomyelitis
- Sepsis and systemic spread
- Chronic joint dysfunction
- Death (especially in elderly or immunocompromised patients)
Prognosis and Outcome
With early diagnosis and proper management, outcomes are generally favorable. Prognosis depends on:
- Promptness of treatment
- Type of causative organism
- Patient’s baseline health and comorbidities
- Adequacy of joint drainage
Delayed treatment significantly increases the risk of irreversible joint damage.
Prevention of Septic Arthritis
- Prompt treatment of systemic infections
- Aseptic techniques during joint injections or surgeries
- Prophylactic antibiotics in high-risk patients undergoing invasive procedures
- Early evaluation of joint pain and swelling in at-risk populations
Special Considerations in Pediatric Septic Arthritis
Children are particularly susceptible to rapid joint damage due to thinner articular cartilage and more vascular metaphysis.
- Hip joint involvement is common
- Requires immediate orthopedic consultation
- Early MRI and surgical drainage often necessary
Septic arthritis is a medical emergency that mandates swift diagnosis and aggressive management. The synergy of clinical suspicion, timely joint aspiration, targeted antibiotics, and appropriate surgical intervention ensures optimal patient outcomes and joint preservation. In high-risk populations, proactive prevention and early recognition remain critical in reducing the morbidity associated with this destructive joint infection.