Sepsis caused by anaerobic bacteria represents a serious medical condition characterized by a dysregulated host response to infection by obligate or facultative anaerobes. These organisms thrive in oxygen-deficient environments such as necrotic tissue, abscesses, and gastrointestinal or genitourinary tracts. Although less frequently isolated in routine cultures, anaerobic pathogens play a critical role in polymicrobial sepsis and carry significant morbidity and mortality if untreated.
Pathogenesis of Anaerobic Sepsis
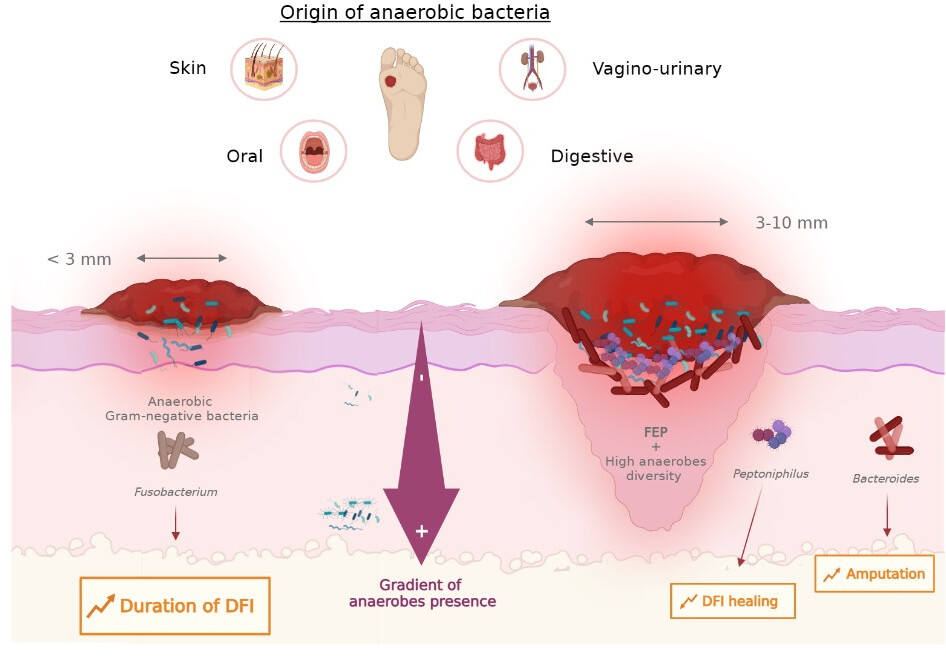
Anaerobic bacteria gain access to the bloodstream through mucosal barrier breaches, surgical wounds, malignancies, or perforated viscera. Once systemic, their pathogenicity is mediated by:
- Endotoxins and exotoxins: Disrupt host immunity and vascular endothelium
- Tissue necrosis: Facilitates local growth and dissemination
- Immune evasion: Capsule formation and reduced immunogenicity
Common Anaerobic Pathogens
| Pathogen | Typical Source | Characteristics |
|---|---|---|
| Bacteroides fragilis | GI tract | Encapsulated, β-lactamase producing |
| Clostridium perfringens | Wounds, gut flora | Gas-forming, exotoxin-producing |
| Fusobacterium spp. | Oropharyngeal | Associated with Lemierre’s syndrome |
| Peptostreptococcus spp. | Skin, GI, GU | Anaerobic cocci, slow-growing |
Risk Factors for Anaerobic Bacteremia
- Abdominal surgeries and perforations
- Malignancy (particularly colorectal and gynecological)
- Immunosuppression (e.g., chemotherapy, corticosteroids)
- Necrotizing soft tissue infections
- Poor dental hygiene or dental procedures
Clinical Manifestations of Anaerobic Sepsis
Anaerobic sepsis often presents insidiously, masking its etiology under a polymicrobial umbrella. Clinical signs include:
- Fever, chills, hypotension
- Tachycardia, leukocytosis
- Organ dysfunction (renal, hepatic, respiratory)
- Signs of localized abscesses (e.g., crepitus, fluctuance)
- Hemolysis in Clostridium perfringens sepsis
Diagnostic Approach to Anaerobic Sepsis
Timely and accurate diagnosis is challenging due to the fastidious nature of anaerobes.
Blood Cultures and Microbiological Identification
- Anaerobic bottles in blood culture sets are essential.
- Slow-growing: May require ≥5 days of incubation.
- MALDI-TOF MS and 16S rRNA sequencing improve identification speed and precision.
Imaging Studies
- CT scans of the chest, abdomen, pelvis to identify abscesses or necrotic tissue
- MRI for soft tissue and spinal infections
Antimicrobial Therapy and Treatment Strategies
Empiric therapy must include coverage for anaerobic pathogens when anaerobic sepsis is suspected.
First-Line Antibiotics
- Metronidazole: Excellent anaerobic coverage; not effective against aerobes
- Beta-lactam/beta-lactamase inhibitors: Piperacillin-tazobactam, ampicillin-sulbactam
- Carbapenems: Imipenem, meropenem for resistant or polymicrobial infections
- Clindamycin: Useful for soft tissue infections; some resistance in Bacteroides noted
Combination Therapy
- Often necessary in polymicrobial infections (e.g., anaerobe + Enterobacterales)
Duration of Treatment
- Uncomplicated bacteremia: 7–10 days
- With abscess or osteomyelitis: 4–6 weeks depending on resolution and site
Surgical and Supportive Management
Source Control
- Percutaneous drainage of intra-abdominal or hepatic abscesses
- Surgical debridement of necrotic tissue or infected prostheses
- Tooth extraction or periodontal management in odontogenic cases
Hemodynamic Support
- Early fluid resuscitation following sepsis protocols
- Vasopressors for persistent hypotension
Monitoring and Follow-Up
- Daily assessment for clinical improvement
- Repeat imaging to ensure resolution of abscesses
- Surveillance cultures if deterioration occurs
Prognosis and Outcomes
Timely initiation of anaerobic-targeted therapy and effective source control significantly improve outcomes. Delays in treatment can result in septic shock, multi-organ failure, and increased mortality.
Mortality Rates
- General anaerobic bacteremia: 15–30%
- Clostridium perfringens sepsis: Up to 70% with hemolysis
- Prognosis worsens with advanced age, immunosuppression, or delayed diagnosis
Challenges and Future Directions
- Underdiagnosis due to insufficient culture techniques
- Antibiotic resistance in anaerobes, especially β-lactamase-producing Bacteroides
- Development of rapid diagnostic platforms for anaerobic pathogens
- Research into anaerobic microbiome interaction and systemic inflammatory responses
Sepsis caused by anaerobic bacteria remains an underrecognized but critical subset of septic presentations. Early suspicion, comprehensive microbiological evaluation, prompt initiation of anaerobic-targeted antibiotics, and definitive source control are vital for reducing morbidity and mortality. Clinicians must maintain a high index of suspicion, particularly in postoperative, immunocompromised, and intra-abdominal infection cases.

