Selective decontamination of the digestive tract (SDD) is an evidence-based prophylactic strategy designed to prevent nosocomial infections in critically ill patients, particularly those in intensive care units (ICUs). It involves the application of non-absorbable antibiotics to the oropharynx and gastrointestinal (GI) tract, often in combination with a short course of systemic antibiotics.
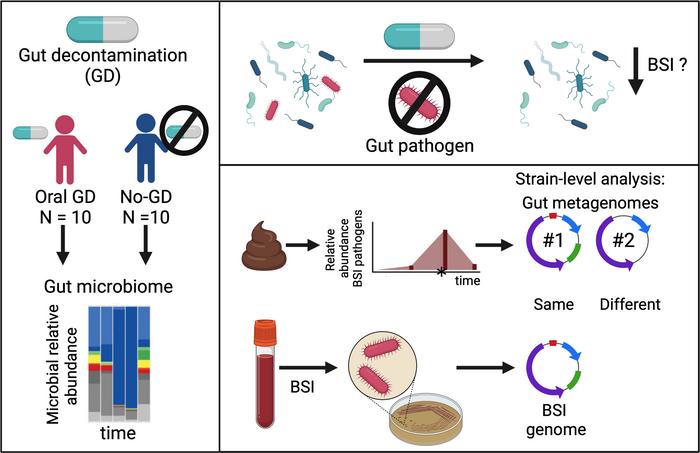
SDD targets potentially pathogenic aerobic bacteria, notably Gram-negative bacilli and Staphylococcus aureus, while sparing the protective anaerobic flora crucial for gut immunity. By reducing the reservoir of pathogens in the digestive tract, SDD aims to decrease the incidence of ventilator-associated pneumonia (VAP), bloodstream infections, and other ICU-acquired infections.
Components of the SDD Protocol
Topical Antibiotic Application
The standard SDD regimen includes:
- Oropharyngeal paste and enteral suspension containing:
- Polymyxin E (colistin)
- Tobramycin or gentamicin
- Amphotericin B (to target Candida spp.)
These agents are administered:
- Every 6 hours via the oropharynx and nasogastric tube
- Throughout the duration of mechanical ventilation or ICU stay
Intravenous Antibiotic Course
A short (usually 4-day) course of systemic antibiotics, typically cefotaxime, is given at the onset of ICU admission to suppress primary endogenous infections.
Microbial Targets and Mechanism of Action
SDD selectively eliminates facultative aerobic Gram-negative bacilli, S. aureus, and yeasts, while sparing strict anaerobes such as Bacteroides species.
Mechanism highlights:
- Suppression of endogenous flora known to translocate during critical illness
- Prevention of secondary colonization by nosocomial pathogens
- Maintenance of gut barrier integrity through anaerobic flora preservation
Clinical Indications and Patient Selection
SDD is most appropriate for:
- Mechanically ventilated ICU patients expected to require prolonged ventilation
- Patients with high risk for sepsis, including trauma, burns, and multi-organ failure
- Settings with high rates of Gram-negative infections
It is not routinely indicated for:
- Immunocompromised individuals (e.g., neutropenic patients)
- Non-ICU or short-stay admissions
- Low-risk patients not receiving mechanical ventilation
Efficacy and Clinical Outcomes of SDD
Ventilator-Associated Pneumonia
Multiple randomized controlled trials (RCTs) and meta-analyses have demonstrated that SDD reduces the incidence of VAP by up to 60%, primarily by preventing early airway colonization.
Bloodstream Infections and Mortality
- SDD significantly lowers bacteremia rates, especially from Enterobacteriaceae
- Some trials report mortality reductions of 10–15% in critically ill populations
ICU Length of Stay
There is evidence that SDD may reduce ICU length of stay due to fewer infectious complications and improved patient stability.
Antimicrobial Resistance: Safety and Surveillance
Resistance Concerns
One of the primary critiques of SDD is the theoretical risk of promoting antibiotic resistance, particularly in high-burden or poorly controlled antimicrobial environments.
However, long-term cohort studies in SDD-using ICUs have shown:
- Stable or reduced antimicrobial resistance rates
- No significant rise in multidrug-resistant organisms (MDROs)
- Preservation of anaerobic flora reduces selection pressure
Surveillance Measures
Routine microbial surveillance is essential to:
- Monitor resistance patterns
- Detect emerging MDROs
- Adjust local protocols based on susceptibility data
Comparison with Selective Oropharyngeal Decontamination (SOD)
SOD involves only oropharyngeal application of non-absorbable antibiotics without gastrointestinal administration.
| Parameter | SDD | SOD |
|---|---|---|
| Application Sites | Oral and gastrointestinal | Oral only |
| Systemic Antibiotics | Yes (initial course) | No |
| Efficacy in VAP Reduction | Superior to SOD in multiple trials | Moderate |
| Resistance Risk | Similar if surveillance is active | Lower theoretical risk |
Implementation Considerations and Protocol Customization
- Antibiotic selection should reflect local microbial flora and resistance profiles
- Standardization of administration through nursing protocols ensures consistent delivery
- Multidisciplinary collaboration involving ICU, pharmacy, microbiology, and infection control teams is vital
Ethical and Regulatory Perspectives
While SDD is standard in several European countries (notably the Netherlands), its adoption remains limited in the United States due to:
- Regulatory hesitancy about off-label antibiotic use
- Institutional antibiotic stewardship policies
- Variability in ICU microbial ecology
Despite these concerns, the strong evidence base warrants serious consideration in ICUs with high infection burdens and robust surveillance infrastructure.
Future Directions and Research
- Precision microbiome-targeted therapies to reduce pathogenic colonization without harming beneficial flora
- Personalized SDD regimens based on rapid microbial diagnostics
- Global surveillance networks to track SDD outcomes and resistance evolution
Selective decontamination of the digestive tract represents a powerful tool in ICU infection control, with robust evidence supporting its efficacy in reducing ventilator-associated pneumonia and bloodstream infections. When implemented with rigorous surveillance and institutional oversight, SDD contributes meaningfully to improved patient outcomes without significantly increasing antimicrobial resistance.

