Intraoperative seizures during neurosurgical procedures represent a critical challenge, with the potential to disrupt surgery, complicate outcomes, and increase morbidity. These events can arise spontaneously or be triggered by surgical stimuli, direct cortical manipulation, or cortical electrical stimulation during brain mapping. An in-depth understanding of their pathophysiology, identification, and immediate intervention strategies is essential for optimizing surgical safety and neurological outcomes.
Etiology of Seizures During Neurosurgery
Direct Cortical Irritation and Stimulation
Mechanical manipulation of the cerebral cortex, particularly in eloquent brain regions, is the most common precipitant. Factors include:
- Resection near epileptogenic zones
- Electrocorticography (ECoG) or direct electrical stimulation during awake craniotomies
- Thermal injury from bipolar cautery
Anesthetic and Pharmacologic Triggers
Certain anesthetic agents lower seizure thresholds:
- Enflurane, sevoflurane, and high doses of etomidate
- Subtherapeutic levels of anticonvulsants in epileptic patients
- Hypoxia, hypercarbia, or electrolyte imbalances intraoperatively
Pre-existing Epilepsy and Structural Lesions
- Tumors, vascular malformations, or traumatic lesions predispose the cortex to hyperexcitability
- Previous seizure history correlates with higher intraoperative seizure risk
Types of Seizures Observed Intraoperatively
- Focal motor seizures: Often induced during awake craniotomy or stimulation mapping
- Generalized tonic-clonic seizures: Less common but potentially catastrophic if unrecognized during general anesthesia
- Electrographic seizures: Detected only on EEG or ECoG, without overt clinical signs under anesthesia
Intraoperative Monitoring and Detection
Role of Intraoperative EEG and Electrocorticography
Electrophysiologic monitoring enables the early identification of seizure activity, especially when clinical observation is limited due to general anesthesia.
Awake Craniotomy Context
During awake procedures, seizure detection relies heavily on patient-reported symptoms (e.g., aura), involuntary movements, or speech arrest. Neuromonitoring teams must remain vigilant to any neurocognitive deviation.
Immediate Intraoperative Seizure Management
Initial Interventions
- Irrigation with Cold Ringer’s Lactate or Saline: Applied directly to cortical surface to abort seizure activity
- Cessation of Stimulation: Temporarily halting brain mapping or manipulation
- Airway Protection: Critical during awake procedures or in conversion to general anesthesia
Pharmacologic Measures
- Midazolam or propofol bolus IV to terminate seizure activity
- Loading doses of antiepileptic drugs (AEDs) such as levetiracetam, phenytoin, or valproate depending on patient history
- Avoiding agents known to exacerbate seizures intraoperatively (e.g., ketamine, high-dose volatile agents)
Prevention Strategies in Neurosurgical Seizure Risk Patients
Preoperative Planning and AED Optimization
- Continuing chronic AEDs up to the morning of surgery
- Preoperative serum level measurement in patients with epilepsy
- Prophylactic loading in high-risk cases
Surgical Techniques to Minimize Risk
- Gentle tissue handling near epileptogenic foci
- Incremental stimulation in cortical mapping
- Using cooled saline irrigation as a preventive tool during cortical dissection
Anesthetic Protocols
- Employ total intravenous anesthesia (TIVA) with propofol and remifentanil in high-risk patients
- Avoid hyperventilation, hypoxia, and hypoglycemia
Postoperative Considerations Following Intraoperative Seizure
Immediate Postoperative Seizure Risk
Patients who seize intraoperatively are at higher risk for early postoperative seizures. Intensive monitoring in a neurocritical care setting is warranted.
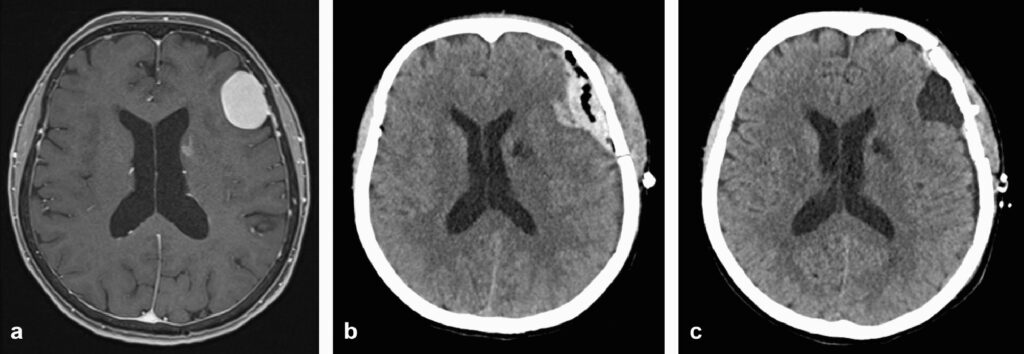
Imaging and Follow-up
- CT or MRI to exclude intracranial hemorrhage, edema, or ischemia
- EEG monitoring in the recovery phase if seizures are suspected
Antiepileptic Therapy Continuation
- Extended AED therapy based on neurologist consultation
- Adjusting regimens based on seizure recurrence and tolerability
Outcomes and Prognostic Implications
While seizures during neurosurgery can be disruptive, prompt identification and management usually prevent long-term complications. However, repeated or prolonged intraoperative seizures may increase the risk of:
- Postoperative neurological deficits
- Cortical injury from prolonged excitotoxicity
- Longer hospital stay and rehabilitation needs
Seizures occurring during neurosurgery present complex intraoperative challenges requiring multidisciplinary awareness and rapid response. The combination of real-time neuromonitoring, effective surgical and anesthetic planning, and immediate intervention protocols ensures patient safety and optimal surgical outcomes. For high-risk patients, preemptive strategies significantly reduce the likelihood of intraoperative seizure episodes and their associated morbidity.

