Sedation, when used as an adjunct to anesthesia, plays a critical role in enhancing perioperative comfort, reducing anesthetic requirements, and optimizing recovery. This approach blends pharmacologic strategies to achieve desired levels of consciousness and analgesia while preserving safety. In many surgical and diagnostic procedures, adjunctive sedation minimizes patient distress, facilitates smoother inductions, and supports anesthetic management.
Clinical Indications for Sedation as an Anesthetic Adjunct
Preoperative Anxiety Management
Sedatives, particularly benzodiazepines, are routinely administered to allay preoperative anxiety. By attenuating stress responses, they reduce sympathetic stimulation, resulting in more stable hemodynamic parameters during induction.
Procedural Cooperation and Tolerance
In regional or neuraxial anesthesia, adjunctive sedation enhances patient cooperation. For procedures involving spinal or epidural blocks, mild to moderate sedation ensures patient immobility and comfort without full unconsciousness.
Reduction in General Anesthetic Requirements
By incorporating sedative-hypnotics or analgesic sedatives, anesthesiologists can lower the dosage of volatile or intravenous anesthetics. This minimizes side effects and supports faster postoperative recovery.
Intraoperative Conscious Sedation
Select procedures—such as those in interventional radiology or vascular surgery—use conscious sedation with local anesthesia. Here, sedation acts as the primary agent while maintaining airway reflexes and cardiorespiratory function.
Pharmacologic Agents Used for Sedation Adjuncts
Benzodiazepines
- Midazolam, Lorazepam
- Provide anxiolysis, amnesia, and sedation
- Used preoperatively and intraoperatively to augment anesthesia
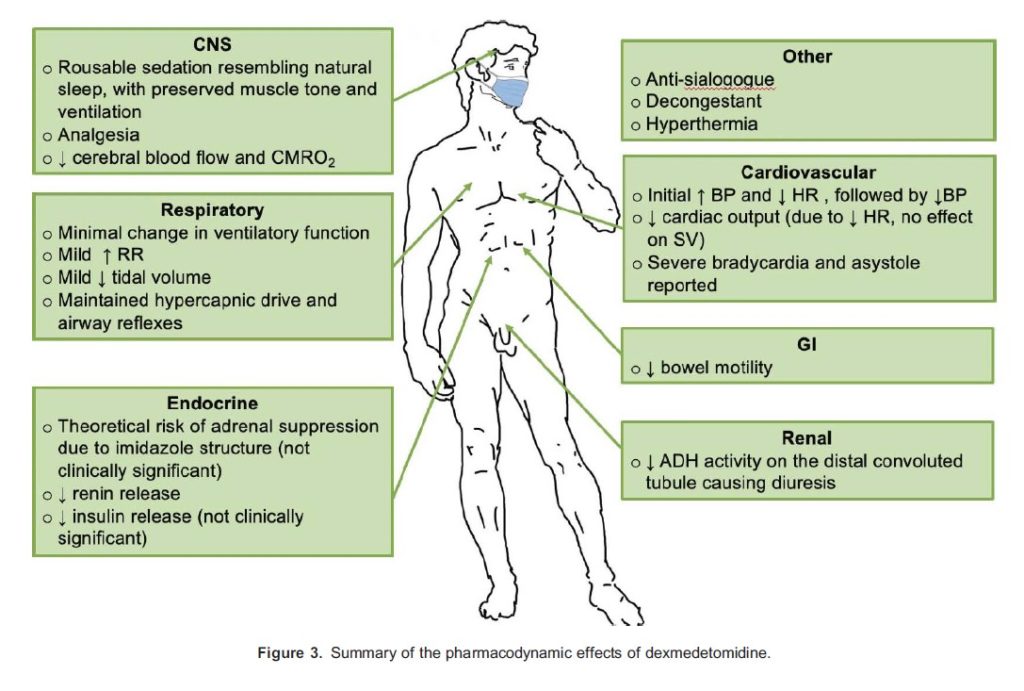
Alpha-2 Adrenergic Agonists
- Dexmedetomidine, Clonidine
- Produce sedation without respiratory depression
- Useful in ICU sedation and during awake fiberoptic intubation
Opioids
- Fentanyl, Sufentanil
- Provide analgesia and mild sedation
- Frequently combined with hypnotics in monitored anesthesia care (MAC)
Propofol
- Short-acting, titratable agent offering both sedation and hypnosis
- Ideal for outpatient procedures and conscious sedation
- Must be administered with airway readiness due to risk of apnea
Ketamine
- NMDA antagonist that induces dissociative anesthesia
- Preserves airway reflexes and is especially valuable in hemodynamically unstable patients
Depth of Sedation: Tailoring for Surgical Requirements
| Sedation Level | Patient Response | Indication in Anesthesia |
|---|---|---|
| Minimal | Normal response to verbal stimuli | Preoperative anxiety, minor adjunct |
| Moderate (Conscious) | Purposeful response to verbal/tactile | MAC, regional blocks, minor surgeries |
| Deep | Response to repeated/painful stimuli | Neurosurgery, pediatric MRI, cardiac catheterization |
| General Anesthesia | Unarousable even with painful stimulus | Major surgery with airway and hemodynamic control |
Monitoring Standards for Sedation-Enhanced Anesthesia
Continuous Clinical Surveillance
- Vital Signs: Blood pressure, respiratory rate, heart rate
- Neurologic Assessment: Responsiveness and verbal communication
- Oxygenation: Pulse oximetry and capnography for respiratory adequacy
- Circulatory Support: ECG monitoring for arrhythmias or ischemia
Sedation Scales for Documentation
- Ramsay Sedation Scale
- Richmond Agitation-Sedation Scale (RASS)
- Observer’s Assessment of Alertness/Sedation (OAA/S)
These scales help quantify sedation levels and guide drug titration intraoperatively.
Advantages of Sedation as an Anesthesia Adjunct
- Enhanced patient satisfaction
- Hemodynamic stability
- Reduced anesthetic dosage
- Faster recovery and discharge
- Decreased postoperative nausea and vomiting (PONV)
- Better pain control in multimodal analgesia strategies
Special Considerations in Sedative-Anesthetic Combinations
Elderly and Frail Patients
Reduced metabolism and increased CNS sensitivity necessitate lower sedative doses. Careful titration avoids delirium, hypotension, or respiratory depression.
Obstructive Sleep Apnea (OSA)
Patients with OSA require meticulous airway monitoring due to elevated risks of hypoxia and apnea during sedative administration.
Pediatric Population
Ketamine and dexmedetomidine are preferred due to their safety profiles in preserving airway tone and preventing emergence agitation.
Procedural Applications of Sedation-Anesthesia Synergy
| Procedure Type | Sedation Role |
|---|---|
| Cataract Surgery | Conscious sedation with local blocks |
| Colonoscopy | Moderate sedation for tolerance and immobility |
| Cardiac Catheterization | Light sedation with continuous hemodynamic monitoring |
| Endovascular Repair | Sedation with spinal/epidural anesthesia |
| Burn Debridement (Pediatric) | Ketamine sedation for analgesia and dissociation |
Recovery and Postoperative Monitoring
Sedation adjuncts should be selected with consideration for rapid offset and minimal residual effects. Key recovery parameters include:
- Airway patency
- Orientation and responsiveness
- Hemodynamic stability
- Pain and nausea assessment
Aldrete scoring is often used to determine readiness for discharge from PACU (Post-Anesthesia Care Unit).
The integration of sedation into anesthetic care has redefined the patient experience and procedural efficiency. When appropriately tailored and monitored, sedation as an adjunct to anesthesia provides a powerful strategy to enhance safety, reduce pharmacologic load, and promote favorable surgical outcomes. Mastery of its pharmacology, patient selection, and monitoring is essential to maximize its benefits across varied clinical contexts.