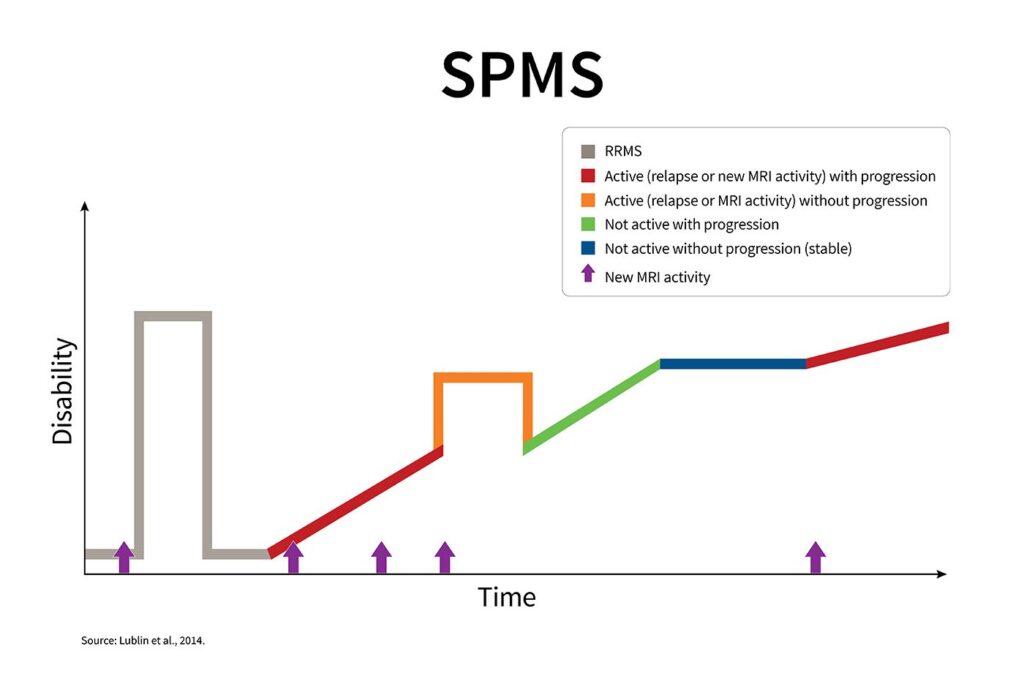
Secondary progressive multiple sclerosis (SPMS) is a distinct phase of multiple sclerosis (MS) characterized by a progressive worsening of neurologic function over time. Initially, patients typically experience a relapsing-remitting course (RRMS), which later transitions into SPMS with or without superimposed relapses. Unlike RRMS, the disease in SPMS gradually advances regardless of inflammation, leading to accumulating disability.
Transition from Relapsing-Remitting MS to SPMS
Defining the Shift
The shift from RRMS to SPMS is subtle and often retrospective. It involves a progressive neurological decline that is independent of acute relapses. Clinically, patients may notice:
- Increasing mobility challenges
- Cognitive decline
- Less recovery after relapses
- Gradual loss of function without overt relapses
This transition typically occurs after 10–20 years of RRMS, although the exact timing varies.
Clinical Features and Symptoms of SPMS
Symptoms of SPMS can be diverse, reflecting the widespread neurological damage typical of advanced MS. Key manifestations include:
- Progressive gait impairment
- Muscle stiffness and spasticity
- Bladder and bowel dysfunction
- Fatigue
- Cognitive impairment
- Sexual dysfunction
- Vision problems
- Depression and mood disturbances
Types of SPMS: Active vs. Non-Active
The latest MS classification distinguishes between:
- Active SPMS: Characterized by ongoing relapses or new MRI lesions
- Non-active SPMS: Marked by slow progression without relapses or MRI activity
Distinguishing between these two is critical for guiding treatment, as disease-modifying therapies (DMTs) are more effective in the active phase.
Diagnosis and Monitoring Progression
Diagnostic Criteria
SPMS diagnosis is based on clinical history and evidence of sustained disability progression. Criteria include:
- Previous RRMS diagnosis
- Gradual worsening over at least 6–12 months
- Exclusion of other causes for decline
Monitoring Tools
- Expanded Disability Status Scale (EDSS): Measures physical disability
- MRI scans: Detect active lesions and atrophy
- Neuropsychological tests: Assess cognitive function
- Patient-reported outcomes (PROs): Capture quality of life and daily function
Treatment of Secondary Progressive MS
While SPMS is more challenging to treat than RRMS, advances in therapy have introduced several options that may slow progression and improve symptoms.
Disease-Modifying Therapies (DMTs)
- Siponimod (Mayzent)
- Approved specifically for active SPMS
- Selective sphingosine-1-phosphate receptor modulator
- Reduces relapse rate and disability progression
- Cladribine and Ocrelizumab
- May be used off-label in some active SPMS cases
- Particularly beneficial for patients with recent MRI activity
- Mitoxantrone
- Rarely used due to cardiotoxicity and leukemia risk
- Reserved for rapidly progressing cases
Symptom Management
- Spasticity: Baclofen, tizanidine, or botulinum toxin
- Fatigue: Amantadine, modafinil
- Bladder dysfunction: Anticholinergics, intermittent catheterization
- Pain and neuropathy: Gabapentin, pregabalin
- Depression: SSRIs or SNRIs
Rehabilitation and Multidisciplinary Care
- Physical therapy: Improves mobility and reduces spasticity
- Occupational therapy: Supports daily functioning and independence
- Speech therapy: Assists with communication and swallowing issues
- Neuropsychological support: Addresses cognitive and emotional symptoms
Lifestyle and Supportive Strategies
Exercise and Physical Activity
Regular, low-impact physical activity enhances strength, flexibility, and cardiovascular health. Tailored exercise plans improve mobility and fatigue.
Nutrition
A balanced diet rich in anti-inflammatory foods (omega-3s, fruits, vegetables, whole grains) may support neurological health, though no specific diet reverses progression.
Mental Health Support
Counseling, support groups, and mindfulness therapies are vital in managing the psychological burden of SPMS.
Emerging Therapies and Research
- BTK inhibitors (e.g., evobrutinib): Modulate B-cell activity and CNS inflammation
- Remyelination therapies: Aim to restore myelin integrity
- Neuroprotective agents: Under investigation for slowing axonal degeneration
- Stem cell therapy: Shows promise in early-phase trials for progressive MS
Continued research holds the potential to revolutionize SPMS management, especially for non-active forms where current options are limited.
Prognosis and Long-Term Outlook
SPMS typically leads to increasing disability over time. However, early detection of transition and prompt initiation of therapy can delay progression. Comprehensive, individualized care improves quality of life and functional outcomes significantly.
Secondary progressive multiple sclerosis represents a complex and evolving phase of MS that demands precise diagnosis, aggressive management, and holistic support. With current therapies and emerging innovations, there is renewed hope for maintaining function, independence, and quality of life in affected individuals.