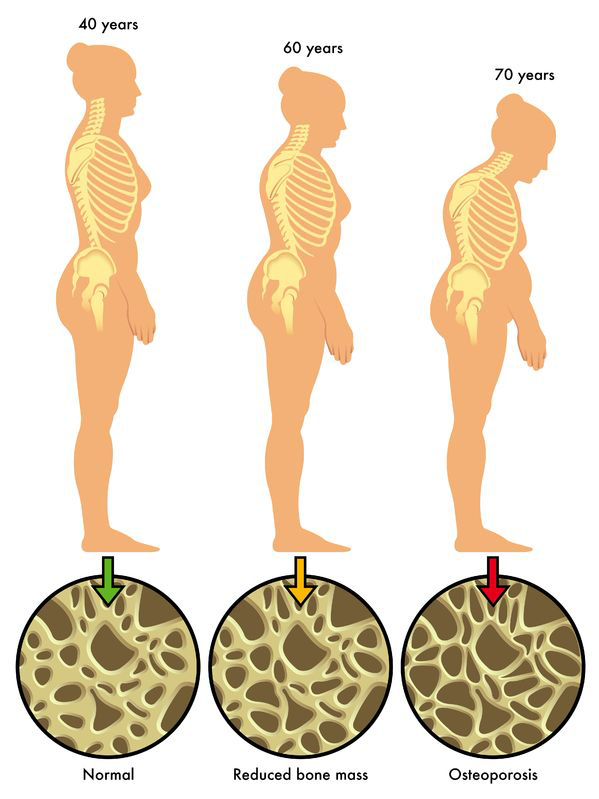
Secondary osteoporosis is a metabolic bone disorder characterized by decreased bone mineral density (BMD) and compromised bone microarchitecture due to identifiable medical conditions or medications. Unlike primary osteoporosis, which is age- or menopause-related, secondary osteoporosis arises from systemic diseases, endocrine imbalances, or pharmacologic agents that accelerate bone loss or impair bone formation. Failure to recognize and address the root cause can result in severe complications, including fragility fractures and prolonged morbidity.
Key Causes of Secondary Osteoporosis
Multiple underlying conditions can trigger secondary osteoporosis by disrupting bone remodeling homeostasis. Identifying the etiology is critical for effective intervention.
1. Endocrine Disorders
- Hyperthyroidism: Increases bone turnover and resorption
- Hyperparathyroidism: Elevates parathyroid hormone, stimulating osteoclastic activity
- Cushing’s syndrome: Excess cortisol weakens bone matrix
- Hypogonadism: Decreased estrogen or testosterone impairs bone formation
2. Gastrointestinal Malabsorption Syndromes
- Celiac disease: Autoimmune damage to intestinal mucosa reduces calcium and vitamin D absorption
- Inflammatory bowel disease: Chronic inflammation and steroid use contribute to bone loss
- Bariatric surgery: Postoperative malabsorption of calcium, vitamin D, and protein
3. Chronic Kidney Disease (CKD)
- Disturbs calcium-phosphorus metabolism
- Secondary hyperparathyroidism and uremia lead to renal osteodystrophy
4. Hematologic and Oncologic Causes
- Multiple myeloma: Malignant plasma cells produce osteoclast-activating factors
- Leukemia and lymphoma: Bone marrow infiltration disrupts normal remodeling
- Bone metastases: From breast, prostate, or lung cancer
5. Medications
- Glucocorticoids: Inhibit osteoblast activity and calcium absorption
- Anticonvulsants: Induce hepatic metabolism of vitamin D
- Aromatase inhibitors and androgen deprivation therapy: Suppress sex hormone production
Bone Loss Mechanism in Secondary Osteoporosis
Secondary osteoporosis results from altered bone remodeling dynamics, favoring resorption over formation. The pathophysiologic mechanisms vary by cause but converge in reduced bone strength and increased fracture risk.
Clinical Features and Risk Indicators
Common Signs and Symptoms
- Fragility fractures (especially vertebral, hip, and wrist)
- Height loss or kyphosis
- Chronic bone pain or tenderness
- Reduced mobility or independence
High-Risk Populations
- Postmenopausal women with comorbidities
- Males under 70 with fractures or chronic diseases
- Long-term corticosteroid users
- Patients with endocrine or gastrointestinal disorders
Diagnostic Evaluation of Secondary Osteoporosis
Early and accurate diagnosis involves assessing bone density and identifying contributory conditions.
1. Bone Mineral Density Testing
- Dual-energy X-ray absorptiometry (DXA): Gold standard
- T-score ≤ -2.5 indicates osteoporosis
2. Laboratory Investigations
- Serum calcium, phosphate, vitamin D, and PTH
- Thyroid function tests
- Sex hormones (testosterone, estradiol, FSH/LH)
- 24-hour urinary calcium
- Markers of bone turnover (e.g., CTX, P1NP)
3. Secondary Workup for Underlying Disease
- Celiac panel, renal function tests, liver enzymes
- Myeloma workup if indicated (SPEP/UPEP, free light chains)
Treatment Approaches for Secondary Osteoporosis
Management targets both skeletal fragility and the underlying etiology. An individualized approach combining pharmacologic therapy, nutritional support, and lifestyle modification yields the best outcomes.
1. Treating the Underlying Condition
- Hormone replacement in hypogonadism
- Control of thyroid or parathyroid disorders
- Gluten-free diet for celiac disease
- Adjustment or discontinuation of bone-depleting medications
2. Pharmacologic Therapy
- Bisphosphonates (alendronate, zoledronic acid): First-line agents
- Denosumab: Effective for glucocorticoid-induced or renal-related osteoporosis
- Teriparatide and Abaloparatide: Anabolic agents stimulating bone formation
- Romosozumab: Dual-action agent—bone formation and resorption inhibition
3. Nutritional and Lifestyle Interventions
- Calcium: 1,000–1,200 mg/day through diet and supplements
- Vitamin D: 800–2,000 IU/day depending on serum levels
- Protein intake: Essential for muscle and bone integrity
- Weight-bearing exercises: Enhance bone strength
- Smoking cessation and alcohol moderation
Complications and Prognosis
Untreated secondary osteoporosis significantly elevates the risk of:
- Vertebral compression fractures
- Hip fractures with high morbidity and mortality
- Chronic pain and reduced quality of life
- Long-term disability and dependence
However, timely diagnosis and treatment can reverse bone loss and prevent complications in many cases.
Monitoring and Long-Term Follow-Up
- DXA scans every 1–2 years to track BMD changes
- Routine blood work to monitor calcium, vitamin D, and bone turnover
- Assess medication adherence and side effects
- Re-evaluate secondary causes if bone loss persists despite therapy
Secondary osteoporosis is a serious yet treatable condition resulting from systemic disorders or medications that disturb bone metabolism. A comprehensive evaluation to identify underlying causes, along with targeted pharmacologic and lifestyle interventions, is essential to prevent fractures and preserve skeletal health. Early detection and ongoing monitoring are key to optimal outcomes.