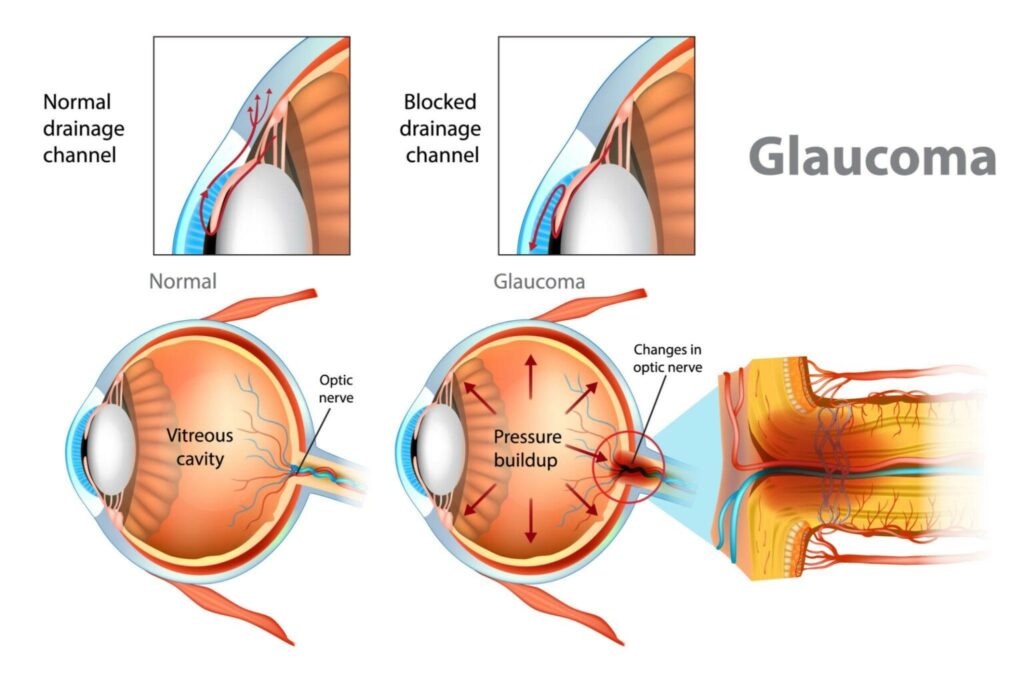
Secondary glaucoma refers to a group of eye disorders characterized by increased intraocular pressure (IOP) due to an identifiable underlying cause. Unlike primary glaucomas, secondary forms result from trauma, inflammation, vascular disorders, medication use, or systemic diseases that impair aqueous humor outflow or increase its production. This progressive optic neuropathy can lead to irreversible vision loss if not promptly addressed.
Key Causes and Classifications of Secondary Glaucoma
Secondary glaucoma is categorized by its underlying etiology, and understanding these subtypes is crucial for targeted treatment.
1. Uveitic Glaucoma
- Occurs in patients with anterior uveitis or panuveitis
- Inflammatory debris and synechiae block trabecular meshwork
- Steroid treatment may paradoxically raise IOP
2. Neovascular Glaucoma
- Caused by abnormal blood vessel growth in the anterior chamber angle
- Common in diabetic retinopathy, central retinal vein occlusion
- Extremely aggressive and resistant to treatment
3. Traumatic Glaucoma
- Results from blunt or penetrating ocular trauma
- Hyphema, angle recession, or intraocular foreign bodies may obstruct outflow
- May develop weeks to years after injury
4. Lens-Induced Glaucoma
- Caused by lens particle release (phacolytic), lens intumescence, or dislocation
- Leads to acute or chronic angle closure
- Often seen post-cataract surgery or trauma
5. Steroid-Induced Glaucoma
- Triggered by topical, systemic, or periocular corticosteroids
- Genetic predisposition affects susceptibility
- Regular IOP monitoring essential for long-term steroid users
6. Pigmentary and Pseudoexfoliation Glaucoma
- Caused by deposition of pigment or fibrillar material in the trabecular meshwork
- More common in older adults
- Requires close monitoring due to rapid progression
Pathophysiology: Mechanism of Increased IOP
Elevated IOP in secondary glaucoma arises either from decreased outflow facility through the trabecular meshwork or increased aqueous humor production. The following diagram illustrates the common pathogenic routes:
Clinical Features and Diagnostic Indicators
Secondary glaucoma presents with variable signs depending on the cause but often includes:
- Elevated intraocular pressure (IOP > 21 mmHg)
- Optic disc cupping
- Visual field defects
- Corneal edema in acute cases
- Eye pain, photophobia, or redness in inflammatory types
Diagnostic Tools:
- Tonometry: Measures intraocular pressure
- Gonioscopy: Assesses angle anatomy and presence of neovascularization or synechiae
- Optical Coherence Tomography (OCT): Evaluates retinal nerve fiber layer
- Visual Field Testing: Detects functional vision loss
- Slit-Lamp Biomicroscopy: Identifies anterior chamber inflammation or hyphema
Advanced Treatment Modalities for Secondary Glaucoma
Management requires treating both elevated IOP and the root cause of glaucoma. Therapy often involves a multidisciplinary approach combining medical, laser, and surgical interventions.
Medical Therapy
- Topical β-blockers: Reduce aqueous humor production
- Prostaglandin analogs: Enhance uveoscleral outflow
- Carbonic anhydrase inhibitors: Lower intraocular pressure
- Alpha agonists: Dual mechanism—decreased production and increased outflow
- Anti-inflammatory agents: In uveitic types, to reduce intraocular inflammation
Note: Steroid use must be cautiously managed to avoid exacerbating IOP elevation.
Laser Treatments
- Laser Peripheral Iridotomy (LPI): For angle closure due to pupillary block
- Cyclophotocoagulation: Reduces ciliary body activity in refractory cases
- Panretinal Photocoagulation (PRP): Used in neovascular glaucoma to reduce ischemia-driven angiogenesis
Surgical Interventions
- Trabeculectomy: Creates an alternate outflow route; gold standard for advanced cases
- Glaucoma Drainage Devices (Ahmed, Baerveldt): Implanted shunts that bypass the trabecular meshwork
- Endoscopic Cyclophotocoagulation: Minimally invasive destruction of ciliary epithelium
- Anterior chamber washout: For hyphema or phacolytic debris
Prognosis and Complications
The prognosis of secondary glaucoma is largely determined by the underlying condition and timeliness of intervention. Delayed diagnosis increases the risk of:
- Permanent optic nerve damage
- Progressive visual field loss
- Blindness
- Recurrent inflammation or angle closure
Close, long-term follow-up is essential to preserve vision and control IOP effectively.
Preventive Measures and Monitoring
- Routine eye examinations for high-risk populations (e.g., diabetics, steroid users)
- Immediate evaluation of ocular trauma
- Tight glycemic control in diabetics to prevent retinal ischemia
- Avoid unnecessary prolonged steroid use
- Regular IOP monitoring during treatment of uveitis or other ocular conditions
Secondary glaucoma represents a serious, vision-threatening consequence of various ocular and systemic disorders. Early detection, accurate identification of the underlying cause, and aggressive management are essential to prevent irreversible vision loss. A comprehensive, tailored approach involving medical, laser, and surgical options ensures optimal outcomes for patients with this complex condition.