Seborrheic dermatitis of the scalp is a chronic inflammatory skin condition that primarily affects sebaceous gland-rich areas, most notably the scalp. It manifests through flaky scales, erythema, itchiness, and greasy patches. The condition is frequently confused with dandruff, which is a milder, non-inflammatory form of seborrheic dermatitis. While not contagious or life-threatening, it often presents as a persistent cosmetic concern and affects quality of life.

Pathogenesis and Underlying Causes
The pathophysiology of seborrheic dermatitis of the scalp involves a multifactorial interaction between host immunity, skin microbiota, and sebaceous gland activity.
Key Contributing Factors:
- Malassezia yeast proliferation: This lipophilic fungus metabolizes sebum, producing fatty acids that irritate the skin, triggering inflammation.
- Sebum overproduction: Excess oil creates a favorable environment for fungal growth and skin barrier disruption.
- Immune dysregulation: A heightened immune response to Malassezia antigens leads to chronic inflammation.
- Genetic predisposition: Individuals with a family history of inflammatory skin conditions are more likely to develop scalp seborrhea.
Triggering and Worsening Factors:
- Cold, dry climates
- Emotional stress
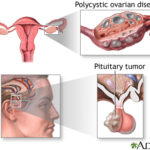
- Hormonal fluctuations
- Infrequent hair washing
- Harsh shampoos or chemical treatments
Clinical Presentation of Scalp Seborrheic Dermatitis
The scalp is the most commonly affected site. Symptoms range in severity and may fluctuate over time.
Common Clinical Features:
- Flaky white or yellowish scales
- Oily, greasy patches on the scalp
- Diffuse or localized redness and irritation
- Itchy, burning sensation
- Exacerbations in winter or during stress
In severe cases, the condition may extend beyond the scalp to the forehead, behind the ears, and along the hairline.
Diagnostic Approach
Diagnosis is typically clinical, based on visual examination of scalp lesions and symptom history. In uncertain cases, further testing may include:
- Microscopy or culture to rule out fungal infections (e.g., tinea capitis)
- Skin biopsy in atypical or treatment-resistant cases
- Dermatoscopy to distinguish from psoriasis or lichen planopilaris
Evidence-Based Treatment Strategies
1. Medicated Shampoos
Medicated shampoos form the foundation of treatment and are applied 2–3 times weekly during flares and once weekly for maintenance.
| Active Ingredient | Mechanism | Common Products |
|---|---|---|
| Ketoconazole | Antifungal | Nizoral, Ketozal |
| Selenium sulfide | Reduces Malassezia & sebum | Selsun Blue |
| Zinc pyrithione | Antifungal & anti-inflammatory | Head & Shoulders Clinical |
| Coal tar | Reduces cell turnover & inflammation | T/Gel |
| Salicylic acid | Keratolytic; removes scales | Denorex, Neutrogena T/Sal |
2. Topical Corticosteroids
For acute inflammation, low to medium potency corticosteroids such as fluocinolone acetonide or clobetasol propionate are applied in lotion or foam formulations. Usage should be limited to 2–4 weeks due to risk of skin atrophy and tachyphylaxis.
3. Topical Calcineurin Inhibitors
Non-steroidal anti-inflammatory agents like tacrolimus and pimecrolimus offer a safer alternative for long-term use, especially in steroid-sensitive areas like the hairline and behind the ears.
4. Systemic Therapy
Reserved for refractory or severe cases, systemic antifungals such as itraconazole or fluconazole are effective in reducing Malassezia density. These are typically prescribed for short durations under specialist supervision.
Long-Term Management and Scalp Care
Daily Maintenance Routine:
- Use medicated shampoo as directed; alternate with mild, non-fragranced shampoos.
- Avoid oil-based styling products which can promote fungal growth.
- Gently massage the scalp during washing to lift and remove scales.
- Rinse thoroughly to prevent residue buildup.
Environmental and Lifestyle Modifications:
- Manage stress through mindfulness or therapy.
- Maintain a balanced diet rich in zinc, vitamin B, and omega-3 fatty acids.
- Limit exposure to extreme temperatures or humidity fluctuations.
- Wash hats, pillowcases, and hair tools frequently.
Differentiating Scalp Seborrheic Dermatitis from Other Conditions
| Condition | Key Differences |
|---|---|
| Psoriasis | Well-demarcated plaques, silver scales, often extends beyond hairline |
| Tinea capitis | Ring-shaped hair loss patches, positive fungal culture |
| Contact dermatitis | Linked to specific allergens or irritants, localized reaction |
| Atopic dermatitis | History of eczema, lichenification, pruritus |
Complications from Untreated Scalp Seborrheic Dermatitis
- Secondary bacterial infections due to scratching
- Hair thinning or telogen effluvium in chronic inflammation
- Psychological distress from cosmetic concerns
- Spread to other sebaceous-rich regions
Prognosis and Outlook
Although seborrheic dermatitis of the scalp is chronic, consistent treatment and lifestyle modifications can result in prolonged remission and minimal flare-ups. With a tailored regimen and proper scalp hygiene, long-term control is achievable for most individuals.
When to Seek Medical Attention
- Lack of response to over-the-counter medicated shampoos
- Severe itching or oozing lesions
- Rapid spreading of symptoms
- Suspicion of other dermatologic or infectious conditions
Seborrheic dermatitis of the scalp is a common yet often misunderstood condition. It results from an interaction between sebum, Malassezia yeast, and an individual’s immune response. Management involves antifungal therapies, inflammation control, and regular scalp hygiene. Through consistent care and appropriate intervention, symptom relief and recurrence prevention are both attainable goals.