Sclerotherapy is a common medical procedure used to treat esophageal varices, particularly in patients with liver cirrhosis. While the procedure is generally effective in controlling variceal bleeding, it can sometimes lead to complications, one of the most significant being sclerotherapy-induced esophageal ulcers. These ulcers can cause severe discomfort and may complicate the patient’s recovery process. In this article, we will delve into the causes, symptoms, diagnosis, treatment options, and prevention strategies for sclerotherapy-induced esophageal ulcers.
Understanding Sclerotherapy and Its Role in Treating Esophageal Varices
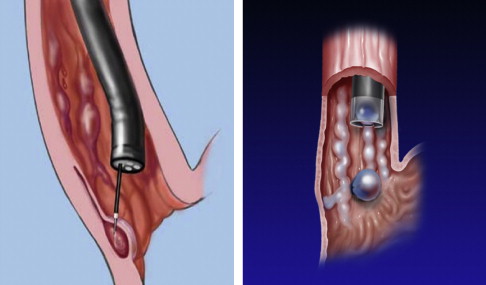
Sclerotherapy is a treatment that involves injecting a sclerosing agent into blood vessels or tissues to induce scarring, which helps control bleeding by sealing off varices. The procedure is commonly used to treat esophageal varices, which are enlarged veins in the esophagus that can rupture, leading to life-threatening bleeding. The sclerosing agents commonly used in esophageal sclerotherapy include sodium tetradecyl sulfate (STS) and polidocanol.
While sclerotherapy can be highly effective, the injection of these chemicals into the esophageal walls can sometimes result in tissue damage, leading to the formation of ulcers. This condition, known as sclerotherapy-induced esophageal ulcers, occurs due to the direct toxic effect of the sclerosing agents or the inflammatory response triggered by the injection.
Causes of Sclerotherapy-Induced Esophageal Ulcer
Sclerotherapy-induced esophageal ulcers are primarily caused by the localized injury resulting from the sclerosing agent injected during the procedure. The main contributing factors to this condition include:
- Chemical Injury: The sclerosing agents, while effective in treating varices, can cause direct chemical injury to the esophageal mucosa, leading to the formation of ulcers.
- Infection Risk: The injection of a foreign substance into the esophageal tissue increases the risk of bacterial infection, which can exacerbate ulcer formation and hinder healing.
- Excessive Injection: Over-injection or incorrect application of the sclerosing agent can cause excessive tissue damage, which may lead to more severe ulcers.
- Esophageal Strictures: In some cases, the formation of ulcers can be accompanied by esophageal strictures, which can further complicate the healing process and lead to chronic symptoms.
Symptoms of Sclerotherapy-Induced Esophageal Ulcer
The symptoms of sclerotherapy-induced esophageal ulcers can vary depending on the severity of the ulcer and its location within the esophagus. Common symptoms include:
- Chest Pain: Patients may experience a burning or sharp pain in the chest, often associated with swallowing or eating.
- Dysphagia: Difficulty swallowing is a common symptom due to the narrowing of the esophagus caused by ulcer formation.
- Heartburn and Regurgitation: The ulceration of the esophageal lining can lead to acid reflux symptoms, including heartburn and regurgitation.
- Bleeding: In severe cases, the ulcer can lead to bleeding, which may present as blood in the vomit or stool.
- Fever and Malaise: These may occur in the presence of infection or as a general inflammatory response to the ulcer.
Diagnosis of Sclerotherapy-Induced Esophageal Ulcer
Diagnosing sclerotherapy-induced esophageal ulcers requires a combination of patient history, clinical examination, and diagnostic procedures. Key diagnostic methods include:
- Endoscopy (EGD): The most definitive diagnostic tool for identifying sclerotherapy-induced ulcers is esophagogastroduodenoscopy (EGD). During this procedure, a flexible scope is inserted through the mouth to visualize the esophagus and stomach. The presence of ulcers, erythema, and other signs of injury can be directly observed.
- Contrast Radiography: In some cases, a contrast-enhanced X-ray may be used to detect esophageal irregularities such as strictures or ulcers.
- Biopsy: In rare cases, a biopsy may be performed to rule out other causes of esophageal ulcers, such as malignancies or infections.
- Patient History: A detailed history of sclerotherapy treatment, including the type and dosage of sclerosing agent used, can provide valuable insights into the likelihood of ulcer formation.
Treatment of Sclerotherapy-Induced Esophageal Ulcer
Treatment for sclerotherapy-induced esophageal ulcers focuses on healing the ulcer and managing symptoms. The treatment approach can be divided into medical and endoscopic interventions:
1. Medical Management
- Proton Pump Inhibitors (PPIs): These medications are used to reduce gastric acid production, providing a less acidic environment to promote ulcer healing.
- Antibiotics: If an infection is suspected or diagnosed, antibiotics may be prescribed to treat the infection and prevent further complications.
- Pain Management: Analgesics such as acetaminophen or opioids may be used to manage pain, though nonsteroidal anti-inflammatory drugs (NSAIDs) should be avoided as they can irritate the ulcer further.
- Nutritional Support: In severe cases, patients may require nutritional support through a feeding tube to ensure adequate intake while the ulcer heals.
2. Endoscopic Therapy
- Endoscopic Hemostasis: In cases where bleeding is present, endoscopic procedures such as coagulation or clipping may be performed to control bleeding and promote healing.
- Dilation: For patients who develop esophageal strictures, endoscopic dilation can help widen the esophagus and alleviate symptoms of dysphagia.
3. Surgical Intervention
In rare cases where ulcers do not respond to conservative treatment, surgical intervention may be necessary to repair the esophagus or remove damaged tissue.
Prevention of Sclerotherapy-Induced Esophageal Ulcer
Preventing sclerotherapy-induced esophageal ulcers is not always possible, but several measures can help reduce the risk of this complication:
- Careful Administration of Sclerosing Agents: Ensuring that the correct dosage and technique are used during sclerotherapy can minimize the risk of excess tissue injury.
- Monitoring: Regular follow-up endoscopies can help detect any signs of ulcer formation early, allowing for prompt intervention.
- Avoiding Overuse of Sclerotherapy: Limiting the number of sclerotherapy sessions and avoiding unnecessary injections can help reduce the likelihood of complications.
- Patient Education: Educating patients about the risks and symptoms of esophageal ulcers can encourage early reporting of symptoms, leading to quicker intervention and better outcomes.
Sclerotherapy-induced esophageal ulcers, while a potential complication of the procedure, can be effectively managed with early diagnosis and appropriate treatment. By understanding the causes, symptoms, and treatment options for these ulcers, healthcare providers can help patients recover more effectively and avoid long-term complications. With careful monitoring and preventive measures, the risks associated with sclerotherapy can be minimized, ensuring optimal patient outcomes.

