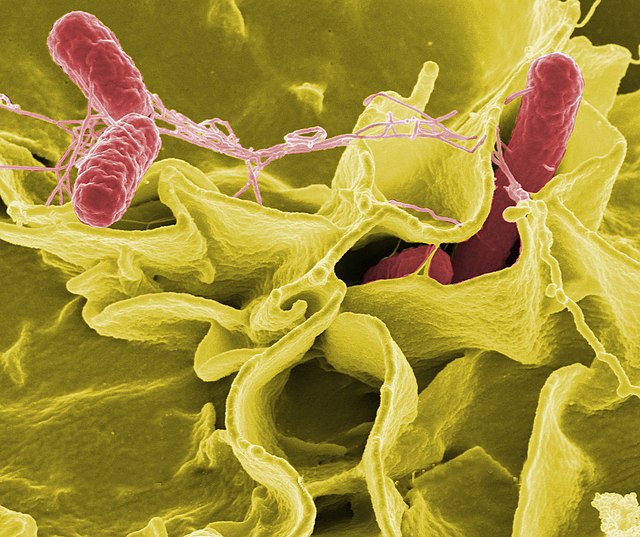
Salmonella septicemia is a serious bloodstream infection caused by the dissemination of Salmonella bacteria beyond the gastrointestinal tract. Unlike localized salmonellosis, which primarily presents as self-limiting gastroenteritis, septicemia involves systemic spread, leading to life-threatening complications if not promptly treated.
This condition typically occurs in immunocompromised individuals, patients with chronic illnesses, or in association with invasive strains like Salmonella enterica serotypes Typhi and Paratyphi. Non-typhoidal salmonella (NTS) can also cause septicemia, particularly in regions with endemic transmission and high HIV prevalence.
Pathogenesis and Risk Factors of Salmonella Bloodstream Infections
Salmonella species are facultative intracellular pathogens that survive and replicate within macrophages. After ingestion, they invade intestinal epithelial cells and Peyer’s patches, breach the mucosa, and enter the reticuloendothelial system, leading to bacteremia.
High-Risk Populations
- Infants and elderly
- Immunosuppressed patients (HIV/AIDS, malignancy, transplant recipients)
- Hemoglobinopathies (e.g., sickle cell disease)
- Chronic liver disease
- Malnourished individuals
Clinical Manifestations of Salmonella Septicemia
The clinical presentation is variable, often mimicking other causes of sepsis or systemic infections.
Common Symptoms
- Prolonged high-grade fever
- Chills and rigors
- Hepatosplenomegaly
- Abdominal pain or discomfort
- Diarrhea or constipation
- Lethargy and malaise
- Rash (rose spots in typhoid fever)
In advanced cases, complications such as septic shock, endocarditis, osteomyelitis, or meningitis may occur, particularly in high-risk groups.
Diagnostic Evaluation of Salmonella Septicemia
Timely and accurate diagnosis is essential to initiate targeted antimicrobial therapy and prevent complications.
Laboratory Investigations
- Blood cultures: Gold standard; multiple samples increase diagnostic yield
- Complete blood count: Leukocytosis or leukopenia, thrombocytopenia
- Liver function tests: Mild transaminitis
- C-reactive protein (CRP) and ESR: Elevated
- Widal test (limited value): May support diagnosis in endemic regions
- Stool and urine cultures: May yield salmonella in systemic dissemination
Imaging
- Abdominal ultrasound or CT scan: Assess for splenic or hepatic abscesses
- Echocardiography: In suspected endocarditis
- Bone scan or MRI: If osteomyelitis is suspected
Antimicrobial Management and Supportive Care
Antibiotic therapy should be guided by local resistance patterns and culture sensitivities. Delay in treatment is associated with increased morbidity and mortality.
First-Line Antibiotics
- Ceftriaxone or cefotaxime (third-generation cephalosporins)
- Azithromycin (especially in enteric fever)
- Fluoroquinolones (e.g., ciprofloxacin) — note increasing resistance
- Meropenem: Reserved for multidrug-resistant strains
Duration of Therapy
- Uncomplicated septicemia: 10–14 days
- Complicated cases (e.g., osteomyelitis): 4–6 weeks
- HIV-associated infections: Extended treatment with consideration for secondary prophylaxis
Supportive Management
- Intravenous fluids for rehydration
- Antipyretics for fever control
- Vasopressors in septic shock
- Monitoring for organ dysfunction
Preventive Measures and Public Health Implications
Individual-Level Prevention
- Safe food handling: Avoid raw or undercooked eggs and poultry
- Hand hygiene: After handling animals or raw food
- Vaccination: Typhoid conjugate vaccines in endemic areas
Community-Level Strategies
- Improved sanitation and clean water supply
- Health education programs
- Surveillance of antibiotic resistance
Complications of Untreated Salmonella Septicemia
Delayed or inadequate treatment can result in severe outcomes:
- Septic shock
- Hepatic and splenic abscesses
- Infective endocarditis
- Septic arthritis or osteomyelitis
- Neurological complications (e.g., meningitis)
Chronic carriers of Salmonella Typhi may contribute to ongoing transmission and should be treated accordingly.
Salmonella septicemia represents a severe manifestation of systemic salmonella infection, demanding prompt recognition, early antimicrobial intervention, and comprehensive supportive care. Risk stratification, judicious diagnostic use, and region-specific treatment strategies are pivotal in reducing associated morbidity and mortality.
In areas with high incidence, aggressive public health initiatives and awareness campaigns are critical to reducing the burden of this potentially fatal condition.