Preterm birth, defined as delivery before 37 weeks of gestation, is a major cause of neonatal morbidity and mortality worldwide. Recurrent preterm birth, which occurs when a woman has experienced a previous preterm delivery, significantly increases the risk of subsequent early deliveries. A history of spontaneous preterm birth is one of the strongest predictors for recurrence, necessitating vigilant prenatal care and tailored preventive interventions.
Etiology and Risk Factors for Recurrent Preterm Birth
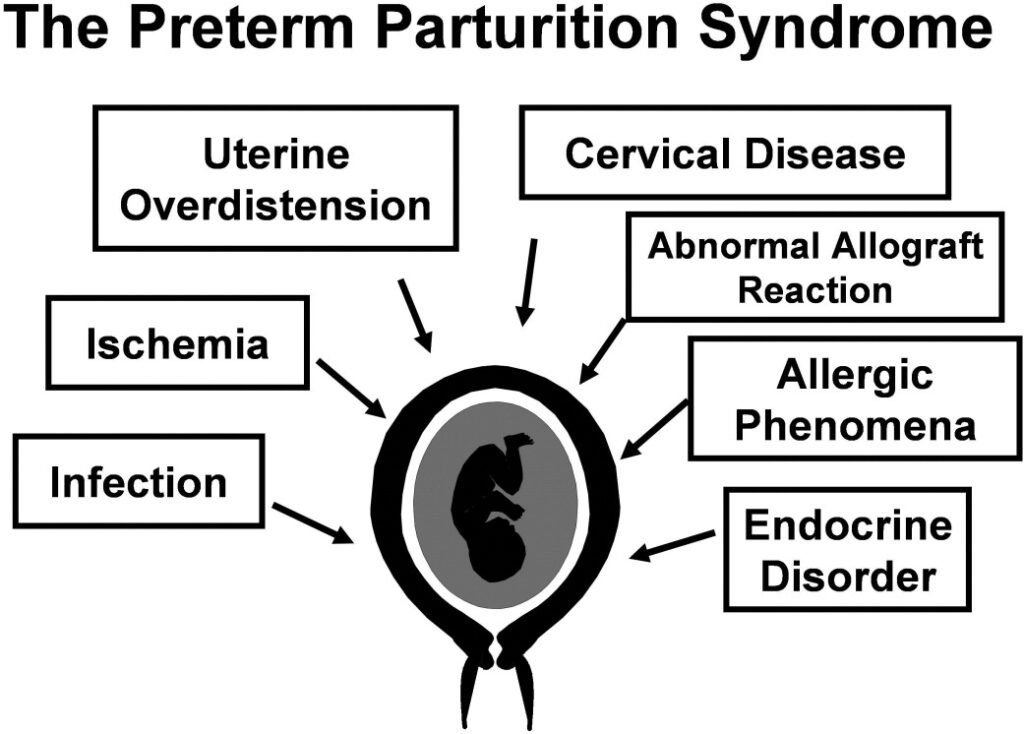
While the precise cause of spontaneous preterm birth often remains multifactorial, several risk factors have been consistently associated with recurrence:
- Prior spontaneous preterm birth
- Short interpregnancy interval (<18 months)
- Cervical insufficiency
- Uterine anomalies
- Infections (e.g., bacterial vaginosis, urinary tract infections)
- Smoking or substance abuse
- Low maternal body mass index (BMI)
- Chronic stress or low socioeconomic status
Evidence-Based Strategies for Risk Reduction
1. Progesterone Therapy
17-alpha hydroxyprogesterone caproate (17-OHPC) is the most commonly used prophylactic therapy in women with a history of spontaneous preterm birth.
- Administration: Weekly intramuscular injection starting between 16 and 20 weeks until 36 weeks.
- Mechanism: Modulates inflammatory pathways and reduces uterine contractility.
- Efficacy: Studies suggest a significant reduction in recurrent preterm birth, particularly in singleton pregnancies.
2. Cervical Length Screening and Cerclage
Transvaginal ultrasound measurement of cervical length is a critical tool in risk stratification.
- Short Cervix (<25 mm): Women with a previous preterm birth and a short cervix benefit from cerclage placement.
- Cerclage Timing: Recommended between 12 and 14 weeks in women with recurrent loss and before 24 weeks in high-risk women with cervical shortening.
- Adjunct Therapy: Vaginal progesterone may be used in women with short cervix and no prior preterm birth.
Optimizing Maternal Health and Lifestyle Factors
1. Smoking Cessation and Substance Use Counseling
Nicotine, alcohol, and illicit drugs have a direct association with uterine irritability and impaired placental function. Smoking cessation programs should be integrated early in prenatal care.
2. Nutritional Optimization
- Folate and Iron Supplementation: Address maternal anemia and neural tube defect prevention.
- BMI Management: Both underweight and obesity have been linked to adverse outcomes. A balanced, nutrient-dense diet supports fetal growth and maternal health.
3. Interpregnancy Interval Management
Evidence suggests a higher risk of recurrent preterm birth in pregnancies spaced <18 months apart.
- Counseling on Contraception: Postpartum contraception should be offered to optimize pregnancy spacing.
- Ideal Interval: 18–24 months between deliveries.
Infections and Inflammatory Triggers
Treating asymptomatic infections reduces systemic inflammation that may trigger preterm labor.
Common Interventions:
- Routine screening for asymptomatic bacteriuria with appropriate antibiotic treatment.
- Treatment of bacterial vaginosis in women with a previous preterm birth and symptoms.
Individualized Care for High-Risk Pregnancies
1. Multidisciplinary High-Risk Clinics
These clinics provide coordinated care involving maternal-fetal medicine specialists, dietitians, behavioral health experts, and social workers.
- Monitoring: Regular fetal growth assessments and biophysical profiles.
- Education: Counseling about early signs of labor and when to seek care.
2. Psychosocial Support and Stress Reduction
Chronic stress and inadequate support networks correlate with adverse pregnancy outcomes. Interventions such as group prenatal care (e.g., CenteringPregnancy) or cognitive-behavioral therapy may improve outcomes.
Role of Tocolytic Therapy and Hospitalization
Although not typically used for long-term prevention, tocolytics may play a role in acute preterm labor management. Routine hospitalization for prevention is not recommended unless complications arise.
Research and Future Directions in Preterm Birth Prevention
Emerging areas of study aim to refine and personalize care for women at risk:
- Biomarkers: Cervicovaginal fetal fibronectin, cytokines, and proteomic profiles under investigation.
- Genomics: Exploring genetic predispositions for preterm birth recurrence.
- Microbiome studies: Understanding the vaginal flora’s role in inflammation and labor initiation.
Risk reduction for recurrent preterm birth requires a comprehensive, evidence-based approach tailored to each patient’s clinical history and risk profile. Progesterone therapy, cervical surveillance, and cerclage are central pillars of care, supplemented by lifestyle optimization, infection management, and psychosocial support. Collaborative and proactive prenatal management is essential to improve neonatal outcomes and reduce the burden of preterm birth on families and health systems.

