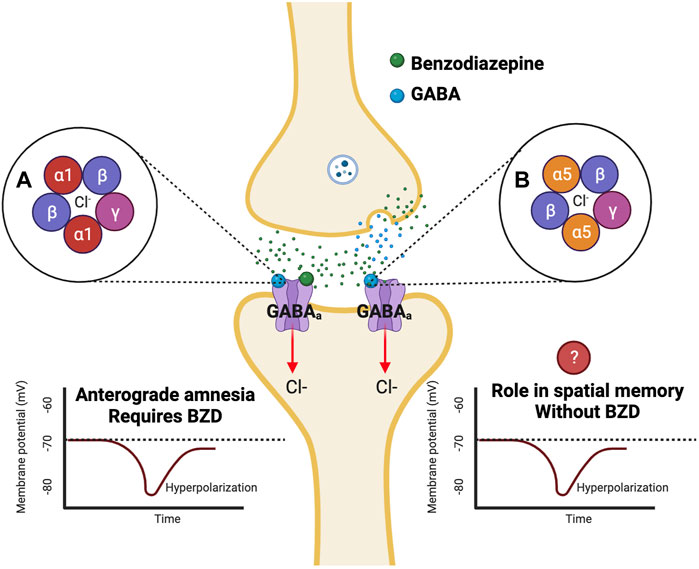
Benzodiazepines are potent central nervous system (CNS) depressants commonly used for anxiolysis, sedation, muscle relaxation, and seizure control. They act on the gamma-aminobutyric acid type A (GABA-A) receptors, enhancing inhibitory neurotransmission and leading to dose-dependent sedation. In cases of overdose or excessive sensitivity, the resulting CNS depression may become life-threatening, necessitating pharmacologic reversal.
Indications for Reversal of Benzodiazepine Sedation
The reversal of benzodiazepine-induced sedation is clinically indicated in specific scenarios, including:
- Severe CNS depression with respiratory compromise
- Overdose involving isolated benzodiazepine ingestion
- Iatrogenic sedation during procedural or ICU care
- Post-anesthesia recovery delays due to benzodiazepine use
- Accidental ingestion, particularly in pediatric or geriatric populations
Flumazenil: The Specific Benzodiazepine Reversal Agent
Mechanism of Action
Flumazenil is a competitive antagonist at the benzodiazepine binding site on the GABA-A receptor. It displaces benzodiazepines and rapidly reverses their sedative effects.
Pharmacokinetics
- Onset: 1–2 minutes
- Peak effect: 6–10 minutes
- Duration: 30–60 minutes
- Half-life: ~40–80 minutes
Due to its short half-life, repeated dosing or continuous infusion may be necessary when reversing long-acting benzodiazepines.
Clinical Dosing Guidelines for Flumazenil
| Clinical Scenario | Initial Dose | Titration | Maximum Dose |
|---|---|---|---|
| Consciousness restoration | 0.2 mg IV over 15 sec | Repeat 0.2 mg at 1-min intervals | 3 mg/hour or 5 mg total |
| Pediatric patients (>1 year) | 0.01 mg/kg IV | Max 0.2 mg/dose | Up to 1 mg/hour |
Continuous infusion may be warranted in cases involving long-acting benzodiazepines like diazepam or clonazepam.
Contraindications and Precautions in Reversal
Flumazenil is not appropriate in every case. Key contraindications include:
- Suspected or known benzodiazepine dependence (risk of seizures or withdrawal)
- Mixed overdose with proconvulsant agents (e.g., tricyclic antidepressants, cocaine)
- History of seizures or epilepsy treated with benzodiazepines
- Elevated intracranial pressure (risk of exacerbation due to abrupt arousal)
Careful patient history, medication review, and risk assessment are essential before administration.
Adverse Effects and Risk Mitigation
While generally well tolerated, flumazenil may cause:
- Seizures, particularly in patients with mixed overdoses or chronic benzo use
- Withdrawal symptoms: agitation, anxiety, tachycardia
- Nausea or dizziness
- Injection site reactions
To reduce risks, clinicians should avoid high bolus doses and perform titration under continuous monitoring.
Monitoring and Supportive Measures
Reversal of sedation must be accompanied by vigilant observation, including:
- Continuous pulse oximetry and capnography
- ECG monitoring for arrhythmias or QT prolongation
- Neurologic assessment every 15–30 minutes post-administration
- Airway support and resuscitative equipment at bedside
When flumazenil wears off, re-sedation may occur, requiring either repeat dosing or supportive ventilation.
Special Considerations in Different Clinical Settings
Procedural Sedation Reversal
- Flumazenil can be administered to expedite patient recovery post-procedure.
- Only appropriate when sedation was achieved solely with benzodiazepines.
- Avoid in patients who received concomitant opioids or have seizure disorders.
ICU Sedation Management
- Used cautiously in weaning protocols where benzodiazepines were part of long-term sedation.
- Gradual dose reduction preferred to abrupt reversal due to risk of delirium and agitation.
Pediatric and Geriatric Populations
- Lower doses with cautious titration due to heightened sensitivity.
- Pediatric reversal must consider developmental differences in metabolism and receptor sensitivity.
Flumazenil Versus Supportive Care Alone
In mild to moderate sedation without respiratory compromise, supportive care with oxygen, fluid resuscitation, and observation may be sufficient. Flumazenil is reserved for:
- Confirmed pure benzodiazepine overdose
- Urgent reversal need (e.g., in conscious sedation settings)
- Failure to respond to conservative management
Alternatives to Pharmacologic Reversal
While flumazenil is the only specific reversal agent, other strategies include:
- Airway management: oxygen therapy, intubation if needed
- Activated charcoal: within 1–2 hours of ingestion if no contraindications
- IV fluids and vasopressors for hypotension
- Close neurologic monitoring until sedative effects subside
Current Guidelines and Recommendations
American College of Medical Toxicology (ACMT):
Recommends flumazenil in highly selected cases—procedural sedation, known naive patients, or iatrogenic overdose.
American Academy of Clinical Toxicology (AACT):
Stresses the importance of risk-benefit assessment prior to reversal.
WHO and EMA:
Support flumazenil for diagnostic use or rapid arousal when clinically justified.
Frequently Asked Questions:
Is flumazenil safe in all benzodiazepine overdoses?
No. It is contraindicated in chronic users or mixed overdoses due to seizure risk.
Can flumazenil reverse all sedative effects immediately?
Flumazenil acts rapidly, but complete reversal depends on the benzodiazepine’s half-life and dose.
Does flumazenil work for alcohol or barbiturate sedation?
No. It is specific to benzodiazepine receptor antagonism and has no effect on other CNS depressants.
How long should patients be monitored after flumazenil use?
At least 2 hours post-final dose, or longer if the ingested benzodiazepine has a long half-life.
What’s the main risk of flumazenil?
Seizures, especially in those with dependence, co-ingestants, or underlying neurologic disorders.
Reversal of benzodiazepine-induced sedation must be approached with precision and caution. While flumazenil offers effective and rapid arousal in appropriate cases, its use is constrained by significant contraindications and potential risks. Thorough patient evaluation, proper dosing, and continuous monitoring are paramount to safe and successful reversal. In settings where flumazenil is not indicated, supportive measures remain the mainstay of management. With informed clinical judgment, sedation reversal can be executed safely to improve patient outcomes.