Apixaban is a direct oral anticoagulant (DOAC) that selectively inhibits factor Xa, thereby preventing thrombin generation and clot formation. It is commonly prescribed for stroke prevention in atrial fibrillation, treatment and prevention of deep vein thrombosis (DVT) and pulmonary embolism (PE). While apixaban offers a predictable pharmacokinetic profile and reduced monitoring requirements, major bleeding or emergency surgery necessitates rapid reversal of its anticoagulant effects.
Indications for Apixaban Reversal
Reversal of apixaban anticoagulation is indicated under specific clinical circumstances, including:
- Life-threatening or major bleeding (e.g., intracranial hemorrhage, gastrointestinal bleeding)
- Urgent surgical interventions where bleeding risk is unacceptable
- Overdose or supratherapeutic levels with signs of coagulopathy
- Trauma or organ rupture in anticoagulated patients
Pharmacokinetics and Clearance of Apixaban
Understanding apixaban’s half-life and elimination pathways informs reversal strategies.
- Half-life: 8 to 14 hours in healthy individuals
- Elimination: Approximately 27% renal, the remainder hepatic and biliary
- Time to offset: Most anticoagulant effect dissipates within 24–48 hours in patients with normal renal function
In cases of impaired renal clearance or high dosing, apixaban may persist longer, increasing bleeding risk.
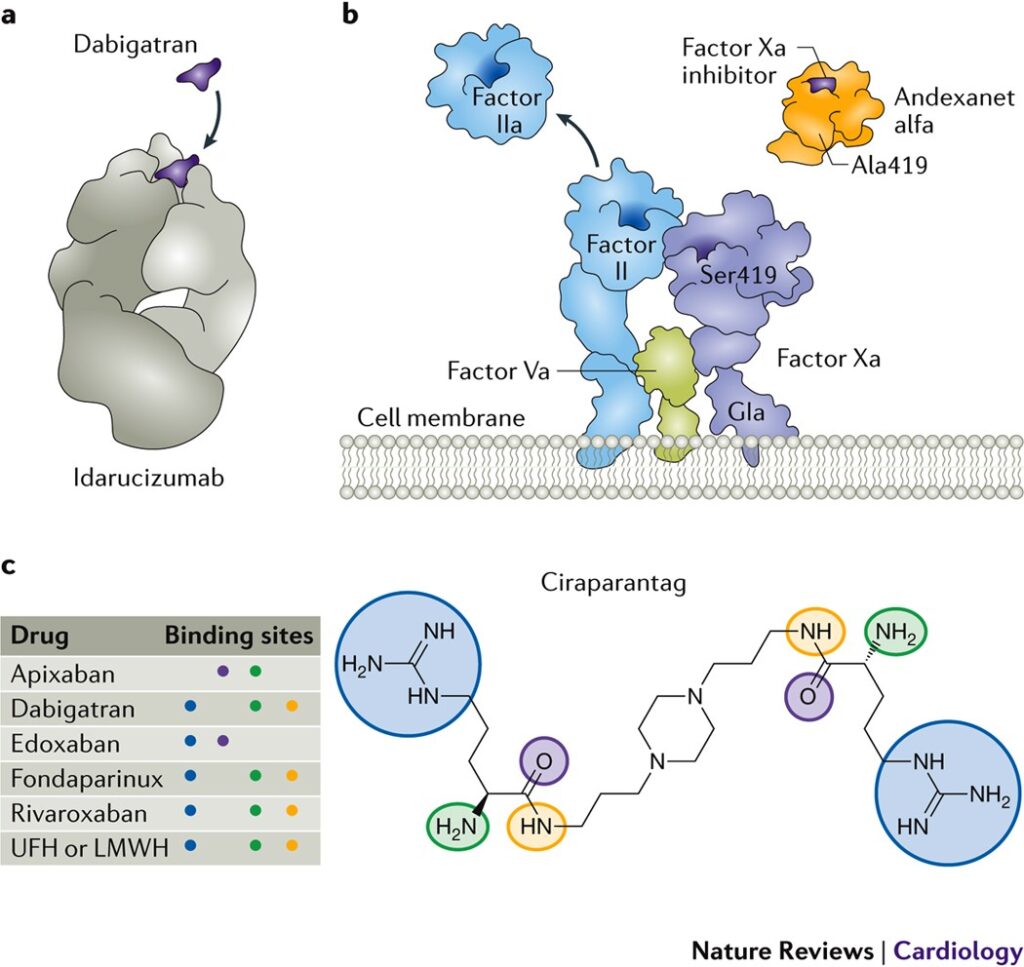
Specific Reversal Agent: Andexanet Alfa
Mechanism of Action
Andexanet alfa is a recombinant modified human factor Xa decoy protein that binds and sequesters apixaban, restoring thrombin generation.
Dosing Protocol
| Clinical Situation | Apixaban Dose | Time Since Last Dose | Andexanet Alfa Regimen |
|---|---|---|---|
| High risk or unknown dose | ≥5 mg | <8 hours or unknown | 800 mg IV bolus + 8 mg/min for 120 min |
| Lower risk | <5 mg | >8 hours | 400 mg IV bolus + 4 mg/min for 120 min |
Efficacy
- Hemostatic effectiveness in up to 80% of major bleeding episodes
- Rapid reversal within minutes of initiation
- Duration of reversal may vary; re-anticoagulation may be necessary
Non-Specific Reversal Strategies
Activated Charcoal
If apixaban ingestion is recent (within 2–6 hours), activated charcoal can reduce absorption.
Prothrombin Complex Concentrates (PCC)
- 4-factor PCCs (e.g., Kcentra) are used off-label
- Dose: 25–50 units/kg IV
- Shown to improve hemostasis but lacks direct neutralization of apixaban
- May be considered if andexanet alfa is unavailable
Hemodialysis
Ineffective for apixaban removal due to high protein binding (~87%) and low dialyzability.
Perioperative Management of Apixaban
Elective Procedures
- Low bleeding risk: Hold 24 hours prior
- High bleeding risk: Hold 48 hours prior
- Resume postoperatively once hemostasis is secured, typically within 24–72 hours
Emergency Surgery
- Administer andexanet alfa or PCC
- Employ local hemostatic measures
- Consider surgical delay if safe and feasible
Laboratory Monitoring
Routine coagulation tests (e.g., PT, aPTT) have limited utility in assessing apixaban activity. Recommended tests include:
- Anti-factor Xa assay (calibrated for apixaban)
- Chromogenic anti-Xa activity (quantitative measurement)
These can confirm therapeutic levels and assist in determining the need for reversal.
Risks and Complications of Reversal
- Thromboembolic events due to reactivation of coagulation
- Hypersensitivity or infusion-related reactions (rare with andexanet alfa)
- Rebound anticoagulation post-reversal requiring reassessment of anticoagulation strategy
Careful monitoring and thromboprophylaxis planning are required post-reversal.
Clinical Considerations and Recommendations
- Assess bleeding severity before initiating reversal
- Balance thrombotic risk against hemorrhagic complications
- Use reversal agents judiciously and in conjunction with surgical or interventional hemostasis
- Reinitiate anticoagulation based on clinical recovery, thrombotic risk, and bleeding resolution
Current Guidelines and Position Statements
American College of Cardiology (ACC)
- Recommends andexanet alfa for life-threatening bleeding
- Supports PCC when specific antidote is unavailable
American Society of Hematology (ASH)
- Emphasizes clinical judgment and individualized approach
- Supports anti-Xa testing to guide decision-making
Emerging Therapies and Research
- Development of universal anticoagulant reversal agents
- Investigation into small molecule antidotes targeting multiple DOACs
- Long-term outcome studies post-reversal are underway to guide safer practices
Frequently Asked Questions:
What is the antidote for apixaban?
Andexanet alfa is the FDA-approved reversal agent for apixaban.
How quickly does andexanet alfa work?
It typically reverses anticoagulation within minutes of administration.
Is PCC effective for apixaban reversal?
Though not FDA-approved for this use, PCC may be beneficial in the absence of andexanet alfa.
Can dialysis remove apixaban?
No. Apixaban is highly protein-bound and not effectively cleared via dialysis.
When can anticoagulation be restarted after reversal?
This depends on bleeding control and thrombotic risk, generally 24–72 hours after stabilization.
Effective management of apixaban reversal requires an understanding of the pharmacology of factor Xa inhibition and a strategic approach to emergencies. While andexanet alfa remains the preferred agent for specific reversal, alternative options such as PCC and supportive care are critical in resource-limited settings. Timely decision-making, guided by clinical severity and laboratory confirmation, ensures optimal outcomes in patients requiring urgent reversal of apixaban anticoagulation.