Retinopathy of prematurity (ROP) is a vasoproliferative disorder of the retina that primarily affects premature infants with low birth weight. Characterized by abnormal development of retinal blood vessels, ROP can lead to retinal detachment and blindness if untreated. With improvements in neonatal care, ROP has become a leading cause of preventable childhood blindness worldwide.
Pathophysiology: How ROP Develops
ROP develops due to disrupted vascular development in the immature retina of preterm infants. The pathogenesis occurs in two main phases:
- Phase I (Vascular Arrest):
After preterm birth, exposure to extrauterine oxygen inhibits normal vascular growth, leading to avascular retina. - Phase II (Neovascularization):
Hypoxia in the avascular retina stimulates abnormal blood vessel proliferation, which can result in fibrovascular tissue, traction, and retinal detachment.
Risk Factors for Retinopathy of Prematurity
Primary Risk Factors
- Gestational age < 32 weeks
- Birth weight < 1500 grams
- Prolonged or unregulated oxygen therapy
Additional Contributing Factors
- Sepsis
- Anemia
- Poor postnatal weight gain
- Mechanical ventilation
- Intraventricular hemorrhage
ROP risk correlates inversely with gestational age and birth weight, making extreme preterm infants especially vulnerable.
Clinical Staging of ROP
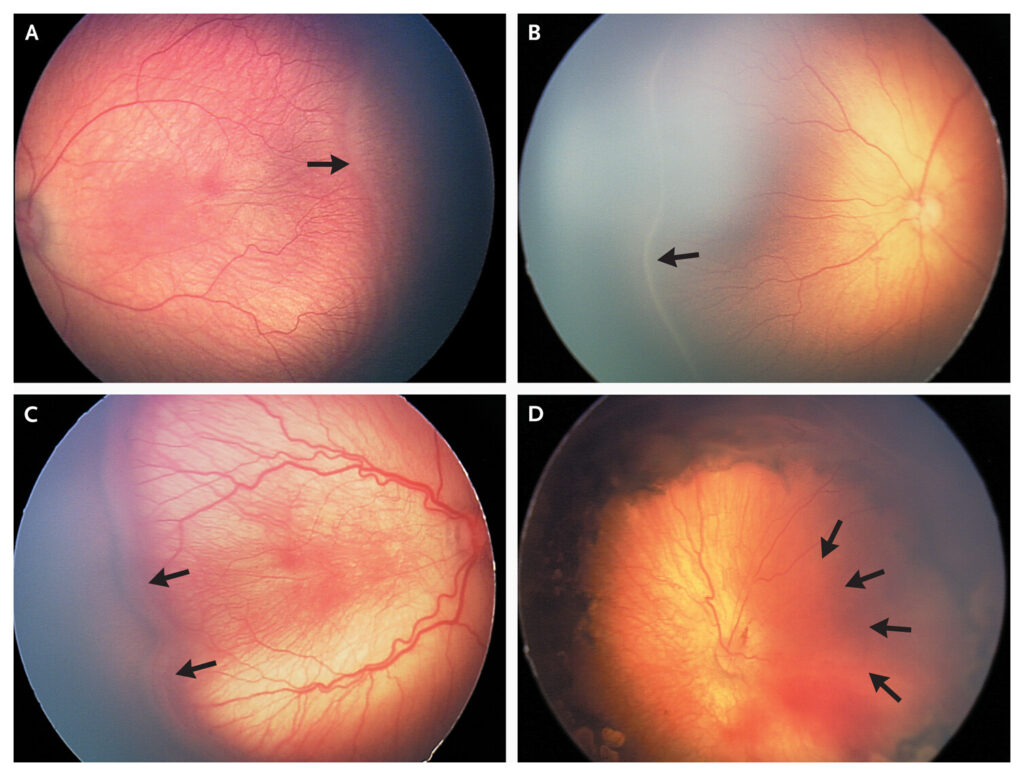
ROP is classified according to the International Classification of Retinopathy of Prematurity (ICROP), which includes:
Stages of ROP
| Stage | Description |
|---|---|
| 1 | Demarcation line between vascular/avascular retina |
| 2 | Ridge with height and width at the junction |
| 3 | Extraretinal neovascularization |
| 4 | Partial retinal detachment |
| 5 | Total retinal detachment |
Zones of Retinal Involvement
- Zone I: Centered on the optic nerve; highest risk zone
- Zone II: Extends from Zone I to the ora serrata nasally
- Zone III: Peripheral crescent-shaped area temporally
Plus Disease
Indicates dilated and tortuous posterior retinal vessels—a marker of severe disease requiring urgent treatment.
Screening Guidelines and Early Detection
Timely screening is vital for detecting ROP before progression to advanced stages.
Recommended Screening Criteria
- Infants born at <30 weeks gestational age
- Birth weight <1500 grams
- Selected infants between 1500–2000 grams with unstable clinical course
Screening Timing
- First exam at 4 weeks chronological age or 31 weeks postmenstrual age (whichever is later)
- Follow-up intervals depend on retinal findings
Treatment Strategies for ROP
Prompt treatment reduces the risk of progression to blindness. Management options depend on disease severity.
Laser Photocoagulation
The gold standard for treating threshold ROP, laser therapy ablates the avascular retina to reduce neovascular stimulus. It preserves central vision but may reduce peripheral fields.
Anti-VEGF Therapy
Intravitreal injections of anti-VEGF agents (e.g., bevacizumab) offer an alternative to laser in Zone I disease. Advantages include:
- Better preservation of peripheral retina
- Reduced myopia risk
However, long-term systemic effects and recurrence rates necessitate close monitoring.
Surgical Management
Advanced stages (4 and 5) may require:
- Scleral buckling
- Pars plana vitrectomy
Surgical success varies, and visual outcomes are often poor once detachment occurs.
Preventive Measures and NICU Protocols
Prevention of ROP begins with optimizing neonatal care practices.
Oxygen Management
- Target SpO₂ levels of 90–95% in premature infants
- Avoid fluctuations in oxygen saturation
Nutrition and Growth Monitoring
- Promote consistent weight gain
- Early initiation of human milk feeding
- Use of growth monitoring as a predictive tool
Infection Control
- Prevent neonatal sepsis
- Judicious use of blood transfusions and antibiotics
Long-Term Outcomes and Follow-Up
Infants treated for ROP require lifelong ophthalmologic monitoring for complications such as:
- Refractive errors (especially myopia)
- Strabismus
- Amblyopia
- Retinal detachment recurrence
Early vision rehabilitation and support services are critical for maximizing functional vision in affected children.
Global Burden and Public Health Impact
ROP is a significant cause of preventable blindness, especially in middle-income countries where neonatal survival is improving but screening programs are inconsistent. A three-tiered approach is necessary:
- Training for neonatologists and ophthalmologists
- Widespread implementation of screening guidelines
- Integration of telemedicine (teleretinal imaging) for remote diagnosis
Frequently Asked Questions:
What is retinopathy of prematurity?
ROP is a disease of the retina that occurs in premature infants, caused by abnormal blood vessel development.
Is ROP reversible?
In mild cases, it may regress spontaneously. Severe stages require treatment to prevent blindness.
At what age should ROP screening begin?
Between 4 weeks of age or at 31 weeks postmenstrual age, depending on birth criteria.
Can ROP be prevented?
While not entirely preventable, risk can be minimized through oxygen regulation and proper neonatal care.
Is anti-VEGF safe for babies?
Anti-VEGF therapy is effective but must be used cautiously due to unknown systemic effects.
Retinopathy of prematurity is a sight-threatening condition that requires a coordinated, evidence-based approach encompassing prevention, early detection, and timely intervention. With proper neonatal protocols and vigilant ophthalmologic care, blindness due to ROP can be significantly reduced, securing a better visual future for vulnerable infants.