Medullary thyroid cancer (MTC) is a rare malignancy arising from parafollicular C-cells of the thyroid, accounting for approximately 3–4% of all thyroid cancers. RET mutations are a defining molecular feature in both hereditary and a significant subset of sporadic MTC cases.
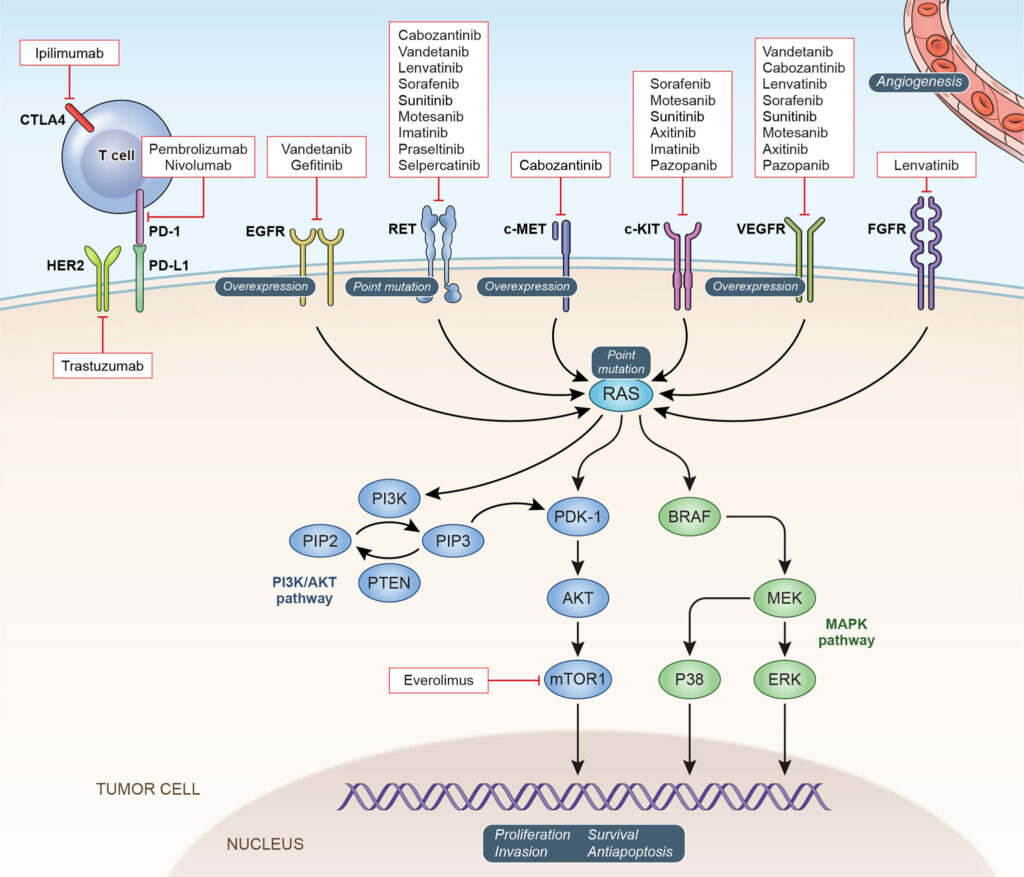
RET-mutant MTC is characterized by constitutive activation of the RET proto-oncogene, leading to dysregulated cell proliferation, differentiation, and survival. Therapeutic approaches targeting this molecular driver have transformed the prognosis and management of advanced disease.
RET Gene and Its Oncogenic Role in MTC
The RET (REarranged during Transfection) gene encodes a receptor tyrosine kinase involved in cell growth and neural crest development. Mutations in RET result in ligand-independent activation, triggering downstream signaling cascades.
Types of RET Mutations in MTC
- Germline RET mutations:
Present in hereditary MTC, including multiple endocrine neoplasia type 2 (MEN2A and MEN2B) syndromes
Common mutations: C634R, M918T, V804M - Somatic RET mutations:
Detected in ~50% of sporadic MTC cases
M918T is the most frequent somatic mutation and correlates with aggressive tumor behavior
These mutations promote oncogenesis through uncontrolled activation of downstream proliferative and anti-apoptotic pathways.
Clinical Presentation and Risk Stratification
Patients with RET-mutant MTC may present with:
- A thyroid nodule or neck mass
- Diarrhea and flushing (from calcitonin secretion)
- Cervical or mediastinal lymphadenopathy
- Metastases in advanced stages (lungs, liver, bone)
Risk Stratification Based on RET Mutations
| RET Mutation | Syndrome Association | Risk Level | Age of Onset |
|---|---|---|---|
| M918T | MEN2B | Highest | Infancy |
| C634R | MEN2A | High | Childhood |
| V804M | FMTC | Moderate | Adulthood |
Risk-adapted management—including prophylactic thyroidectomy in hereditary cases—depends on the mutation type and penetrance.
Diagnostic Approach to RET-Mutant MTC
Early detection and precise mutation identification are essential for optimal management.
Biochemical Markers
- Serum calcitonin: Marker of tumor burden
- Carcinoembryonic antigen (CEA): Correlates with disease progression
Genetic Testing
- Germline RET testing: Mandatory in all MTC cases
- Somatic RET mutation analysis: For sporadic cases using NGS panels
Imaging and Staging
- Ultrasound: Initial thyroid and nodal assessment
- CT/MRI: For locoregional extension
- PET-CT or MIBG scans: Evaluate metastatic spread
- Bone scans: If bone metastasis suspected
Targeted Therapies for RET-Mutant Medullary Thyroid Cancer
Selpercatinib (LOXO-292)
- Selective RET inhibitor approved for advanced RET-mutant MTC
- High objective response rate (ORR > 70%)
- Effective in both treatment-naïve and pretreated patients
- Crosses blood-brain barrier, addressing CNS metastases
- Common side effects: dry mouth, hypertension, liver enzyme elevation
Pralsetinib (BLU-667)
- Potent RET kinase inhibitor approved for RET-mutant MTC
- Shows durable responses and significant reduction in tumor burden
- Used in patients with resistance to multikinase inhibitors
- Side effects: fatigue, neutropenia, constipation
These agents have drastically improved survival and quality of life, with median progression-free survival exceeding 18–20 months.
Comparison to Traditional Multikinase Inhibitors
Prior to RET-specific agents, treatment relied on multikinase inhibitors (MKIs) such as:
- Vandetanib
- Cabozantinib
These agents also target VEGFR, EGFR, and RET but are associated with higher toxicity due to off-target effects. RET-selective inhibitors offer:
- Higher specificity
- Improved tolerability
- Enhanced intracranial activity
- Greater duration of response
Mechanisms of Resistance and Future Directions
Despite initial success, resistance may develop due to:
- Gatekeeper mutations (e.g., RET V804M/L)
- Solvent front mutations (e.g., G810R/S/C)
- Activation of bypass pathways (e.g., RAS, MET amplification)
Investigational Approaches
- Next-generation RET inhibitors (e.g., TPX-0046)
- Combination therapies with MEK or MET inhibitors
- Immunotherapy in tumors with high tumor mutational burden
Clinical trials are ongoing to evaluate adaptive resistance strategies and long-term outcomes.
Prognosis and Long-Term Monitoring
RET mutation status plays a crucial role in predicting prognosis. Patients with M918T mutations have the most aggressive disease and worst outcomes, while V804M mutations carry a more indolent course.
Surveillance Strategy
- Calcitonin and CEA levels every 3–6 months
- Imaging every 6–12 months depending on disease burden
- Monitoring for cardiovascular, hepatic, and renal toxicity related to targeted therapies
Proactive follow-up ensures early detection of recurrence and optimal management of therapy-related adverse effects.
Frequently Asked Questions:
What is RET-mutant medullary thyroid cancer?
A type of thyroid cancer driven by mutations in the RET gene, often aggressive but responsive to targeted therapy.
Are RET mutations hereditary?
Yes, especially in MEN2 syndromes. All MTC patients should undergo germline RET mutation testing.
How is RET-mutant MTC diagnosed?
Through genetic testing, serum calcitonin/CEA levels, and advanced imaging techniques.
Can RET-mutant MTC be cured?
Early-stage disease may be curable with surgery. Advanced cases benefit from targeted therapy for prolonged survival.
What are the latest treatments?
Selective RET inhibitors—selpercatinib and pralsetinib—offer high response rates and are now standard of care.