Renal tubular acidosis (RTA) is a disorder of the kidneys that results in an accumulation of acid in the body. This condition occurs when the kidneys are unable to effectively excrete acid or reabsorb bicarbonate, leading to a chronic state of metabolic acidosis. The inability to properly balance acids and bases in the blood can cause significant health complications. RTA can be classified into different types based on the area of the kidney affected, and its management involves addressing both the underlying cause and the symptoms. In this article, we will explore the causes, symptoms, diagnosis, and treatment strategies for renal tubular acidosis.
What is Renal Tubular Acidosis?
Renal tubular acidosis refers to a group of disorders where the kidneys fail to adequately acidify the urine, causing a build-up of acid in the bloodstream. The kidneys are responsible for maintaining the body’s pH balance by excreting excess hydrogen ions (acid) and reabsorbing bicarbonate (a base) from urine. When this process is disrupted, it can lead to metabolic acidosis, a condition characterized by an overly acidic pH in the blood.
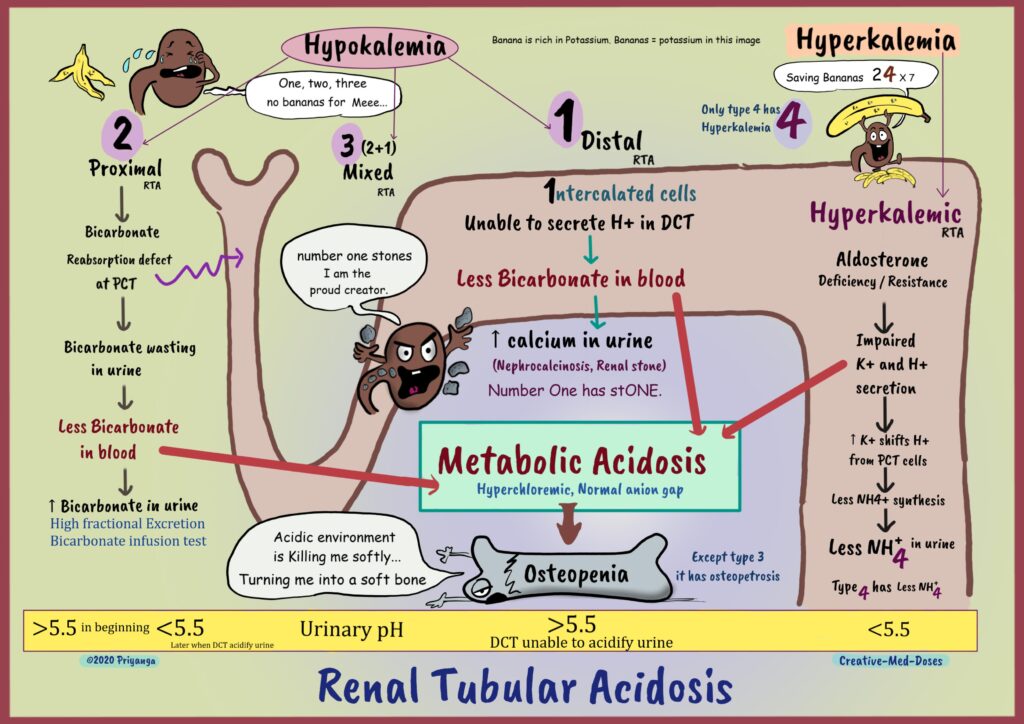
There are three primary types of renal tubular acidosis, each affecting different parts of the kidney:
- Type 1 – Distal Renal Tubular Acidosis (dRTA)
- Type 2 – Proximal Renal Tubular Acidosis (pRTA)
- Type 3 – Mixed or Combined RTA
Causes of Renal Tubular Acidosis
The causes of renal tubular acidosis vary depending on the type of RTA. Here, we break down the causes for each type:
1. Distal Renal Tubular Acidosis (dRTA)
dRTA occurs when the distal tubules of the kidneys cannot effectively excrete hydrogen ions, leading to an acidic environment in the blood. Causes of dRTA include:
- Autoimmune diseases: Conditions like Sjögren’s syndrome, lupus, and rheumatoid arthritis can affect kidney function and lead to RTA.
- Medications: Certain drugs, including lithium and amphotericin B, can damage the distal tubules.
- Genetic mutations: Hereditary forms of dRTA can occur due to mutations in genes that affect hydrogen ion excretion.
- Chronic kidney disease: Kidney damage resulting from diabetes or hypertension can result in impaired kidney function.
2. Proximal Renal Tubular Acidosis (pRTA)
pRTA involves the inability of the proximal tubules to reabsorb bicarbonate, resulting in loss of this important base and an increase in blood acidity. Causes of pRTA include:
- Inherited disorders: Fanconi syndrome, a genetic disorder that affects the proximal tubule, is a common cause of pRTA.
- Acquired conditions: Conditions like multiple myeloma, vitamin D deficiency, and kidney transplantation can lead to pRTA.
- Medications: Drugs such as ifosfamide, tenofovir, and certain diuretics can damage the proximal tubules and cause pRTA.
3. Mixed or Combined Renal Tubular Acidosis
In some cases, patients may experience both distal and proximal tubular dysfunction, leading to a mixed form of RTA. This can occur due to various genetic disorders, chronic kidney diseases, or systemic conditions like metabolic acidosis.
Symptoms of Renal Tubular Acidosis
The symptoms of renal tubular acidosis are primarily related to the underlying acid-base imbalance and its effects on the body. These can vary depending on the type of RTA but commonly include:
- Fatigue and weakness: Persistent metabolic acidosis can result in a general feeling of tiredness and muscle weakness.
- Bone pain: The loss of calcium from bones due to acidic blood can lead to bone demineralization and discomfort.
- Growth retardation: In children, RTA may stunt growth due to impaired calcium and phosphate metabolism.
- Kidney stones: Excess calcium in the urine can lead to the formation of kidney stones, which may cause pain and blockages.
- Polyuria and polydipsia: Increased urination and thirst are common as the kidneys attempt to excrete excess acid.
- Hypokalemia: Low potassium levels may develop, especially in patients with dRTA.
Diagnosis of Renal Tubular Acidosis
Diagnosing renal tubular acidosis involves a combination of clinical evaluation, laboratory tests, and imaging studies. The key diagnostic tools for RTA include:
- Blood tests: Blood gas analysis will reveal metabolic acidosis, characterized by a low blood pH and bicarbonate levels. An elevated anion gap may indicate the presence of other acid-base imbalances.
- Urine pH: A urine pH greater than 5.5, despite metabolic acidosis, is indicative of RTA, particularly in type 1.
- Serum electrolytes: Blood tests showing low potassium levels (hypokalemia) may suggest dRTA, while abnormalities in phosphate and calcium levels are indicative of pRTA.
- 24-hour urine collection: This can assess the kidney’s ability to excrete acid and bicarbonate, further helping to differentiate between types of RTA.
- Imaging: X-rays or CT scans may be performed to check for kidney stones or other renal abnormalities.
Treatment of Renal Tubular Acidosis
The treatment of renal tubular acidosis focuses on correcting the acid-base imbalance, managing electrolyte disturbances, and preventing complications such as kidney stones and bone demineralization. Key treatment options include:
1. Bicarbonate Therapy
The primary treatment for RTA is the administration of sodium bicarbonate or potassium citrate, which helps neutralize the excess acid in the body. This treatment aims to restore the body’s pH balance and prevent further damage to the kidneys and bones.
2. Potassium Supplementation
Many patients with RTA, particularly those with dRTA, develop hypokalemia (low potassium levels). Potassium supplements are often required to maintain appropriate potassium levels and prevent further complications like muscle weakness or arrhythmias.
3. Phosphate and Calcium Supplements
In cases where RTA causes bone demineralization, calcium and phosphate supplements may be prescribed to support bone health and prevent fractures. This is particularly important in pediatric patients, where growth and bone development may be affected.
4. Dialysis
In severe cases of RTA, especially when the kidneys are significantly damaged, dialysis may be required to remove excess acid from the bloodstream and restore the body’s electrolyte balance.
5. Treating the Underlying Cause
In some cases, the underlying condition contributing to RTA (such as autoimmune diseases or chronic kidney disease) will also need to be addressed. Treatment may involve the use of immunosuppressive medications or management of kidney disease to slow its progression.
Prevention and Lifestyle Modifications
While RTA is often caused by genetic factors or chronic diseases, certain lifestyle changes can help manage the condition and prevent complications:
- Maintaining proper hydration: Staying well-hydrated helps the kidneys function more effectively and reduces the risk of kidney stone formation.
- Monitoring kidney function: Regular check-ups with a healthcare provider can help identify early signs of RTA and prevent progression to more severe kidney damage.
- Balanced diet: A diet rich in fruits, vegetables, and low in processed foods can help support kidney function and minimize complications related to RTA.
- Avoiding nephrotoxic medications: Patients with RTA should avoid medications that can further damage the kidneys, such as nonsteroidal anti-inflammatory drugs (NSAIDs) and certain antibiotics.
Renal tubular acidosis is a complex disorder that affects the kidney’s ability to maintain acid-base balance, leading to metabolic acidosis and a range of complications. Understanding the different types of RTA, their causes, symptoms, and treatment options is essential for effective management. Through early diagnosis, appropriate treatment strategies, and lifestyle modifications, patients with RTA can manage their condition and prevent long-term damage to the kidneys and bones.