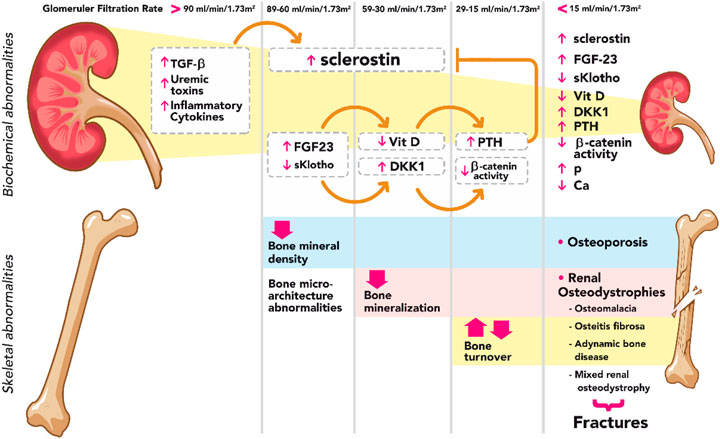
Renal osteodystrophy is a term that refers to bone disease associated with chronic kidney disease (CKD). One of the most critical components of this condition is hyperphosphatemia, an abnormally high level of phosphate in the blood, which plays a significant role in the development and progression of renal osteodystrophy. When kidney function declines, the ability to regulate phosphate and other minerals such as calcium and vitamin D is impaired, contributing to bone abnormalities, fractures, and other skeletal complications. In this article, we will explore the relationship between renal osteodystrophy and hyperphosphatemia, providing an in-depth look at the causes, symptoms, diagnostic methods, and treatment strategies for managing this condition.
Understanding Hyperphosphatemia and Its Role in Renal Osteodystrophy
Hyperphosphatemia occurs when there is an excess of phosphate in the bloodstream, typically due to the kidneys’ inability to excrete phosphate properly. Phosphate is a vital mineral that is necessary for the formation of bones and teeth, but excessive levels can lead to adverse health effects, particularly in individuals with CKD. Elevated phosphate levels can cause calcification of soft tissues, such as blood vessels, as well as bone demineralization, contributing to renal osteodystrophy.
Key Mechanisms of Hyperphosphatemia:
- Decreased Renal Excretion: As kidney function declines in CKD, the kidneys’ ability to filter and excrete phosphate diminishes, leading to increased levels of phosphate in the blood.
- Impaired Phosphate and Calcium Balance: Hyperphosphatemia disrupts the balance between phosphate and calcium, leading to altered bone metabolism.
- Secondary Hyperparathyroidism: Elevated phosphate levels stimulate the parathyroid glands to produce excessive parathyroid hormone (PTH), which further contributes to bone resorption and the weakening of bones.
Causes and Risk Factors of Renal Osteodystrophy with Hyperphosphatemia
The primary cause of renal osteodystrophy with hyperphosphatemia is the inability of the kidneys to properly manage phosphate and other minerals in patients with CKD. As kidney function deteriorates, phosphate excretion becomes impaired, and levels in the blood rise. Other factors that contribute to this condition include:
- Chronic Kidney Disease (CKD): The primary condition leading to hyperphosphatemia and renal osteodystrophy is CKD. With reduced glomerular filtration rate (GFR), phosphate retention increases, triggering secondary complications.
- Dietary Phosphate Intake: A high-phosphate diet, often found in processed foods, can exacerbate the condition by increasing the body’s phosphate burden.
- Medications and Supplements: Certain medications, such as phosphate-containing supplements or medications that affect calcium and phosphate metabolism, may increase the risk of hyperphosphatemia.
- Vitamin D Deficiency: The kidneys are responsible for converting vitamin D into its active form. In CKD, this function is impaired, which can further contribute to calcium and phosphate imbalances.
Symptoms of Renal Osteodystrophy with Hyperphosphatemia
Renal osteodystrophy with hyperphosphatemia presents with a range of symptoms, many of which are related to bone and mineral abnormalities. Key symptoms include:
- Bone Pain and Tenderness: Individuals may experience discomfort, swelling, or tenderness in the bones and joints, particularly in the lower back, ribs, and legs.
- Bone Deformities: Weakened bones due to the loss of calcium and the effects of hyperphosphatemia may result in bone deformities or fractures.
- Itching: Elevated phosphate levels often cause severe itching, a common symptom for patients with hyperphosphatemia.
- Fractures: Due to decreased bone density, fractures may occur even with minimal trauma or injury.
- Growth Retardation in Children: In pediatric patients, renal osteodystrophy can cause growth retardation and delayed bone development.
Diagnosis of Renal Osteodystrophy with Hyperphosphatemia
The diagnosis of renal osteodystrophy with hyperphosphatemia involves several diagnostic steps, including blood tests, imaging studies, and clinical evaluations. Key diagnostic methods include:
- Blood Tests: Measurement of serum phosphate, calcium, PTH, and vitamin D levels are essential for assessing the mineral balance and diagnosing hyperphosphatemia.
- Bone Biopsy: A bone biopsy may be performed in some cases to directly assess the degree of bone involvement and the extent of renal osteodystrophy.
- X-Rays and Imaging Studies: Imaging tests, such as X-rays or bone scans, can identify bone demineralization, fractures, and soft tissue calcification associated with renal osteodystrophy.
- Dual-Energy X-ray Absorptiometry (DEXA) Scan: This scan is used to measure bone density and detect osteoporosis or osteopenia, which are commonly observed in patients with renal osteodystrophy.
Treatment Strategies for Renal Osteodystrophy with Hyperphosphatemia
Effective treatment for renal osteodystrophy with hyperphosphatemia focuses on managing hyperphosphatemia, improving bone health, and addressing the underlying kidney disease. Treatment options include:
1. Phosphate Binders
Phosphate binders are the cornerstone of treatment for hyperphosphatemia in CKD. These medications help reduce the absorption of phosphate from the gastrointestinal tract, thereby lowering phosphate levels in the blood.
- Calcium-Based Phosphate Binders: These are commonly used to control phosphate levels but should be used cautiously to avoid increasing blood calcium levels.
- Non-Calcium-Based Phosphate Binders: For patients at risk of hypercalcemia, non-calcium-based binders, such as sevelamer, are often preferred.
2. Vitamin D Therapy
Vitamin D plays a vital role in calcium and phosphate metabolism. Patients with CKD often require vitamin D supplementation to help manage calcium absorption. Active vitamin D analogs, such as calcitriol, may also be prescribed to reduce PTH levels and improve bone health.
3. Dialysis Management
For patients undergoing dialysis, managing phosphate levels is essential. Dialysis removes excess phosphate from the bloodstream, but phosphate binders and other therapies may still be needed to control phosphate levels.
4. Parathyroidectomy
In cases of severe secondary hyperparathyroidism, surgical removal of the parathyroid glands (parathyroidectomy) may be necessary to control excessive PTH secretion and prevent further bone damage.
5. Dietary Management
A low-phosphate diet is essential for patients with CKD. Reducing the intake of phosphate-rich foods such as dairy products, processed meats, and soft drinks can help manage hyperphosphatemia.
Prevention and Lifestyle Modifications
Preventing renal osteodystrophy with hyperphosphatemia involves early detection and effective management of kidney disease. Some lifestyle modifications include:
- Adhering to a Low-Phosphate Diet: Patients should limit foods high in phosphate and work with a dietitian to ensure proper nutrition.
- Monitoring Kidney Function: Regular blood tests to monitor kidney function, phosphate levels, and PTH levels are essential for managing the condition.
- Avoiding Smoking and Excessive Alcohol: Both smoking and alcohol can worsen kidney function and contribute to mineral imbalances.
Renal osteodystrophy with hyperphosphatemia is a complex and debilitating condition that arises due to kidney dysfunction, leading to abnormal phosphate metabolism and bone health deterioration. Early diagnosis and targeted treatment, including phosphate binders, vitamin D supplementation, and dietary adjustments, can significantly improve the quality of life for individuals with chronic kidney disease. Effective management of hyperphosphatemia and the underlying kidney disease can help reduce bone damage, prevent fractures, and improve overall bone health in affected patients.