Relapsing form of multiple sclerosis (RMS) refers to a neurological condition characterized by clearly defined attacks of new or increasing neurologic symptoms. These relapses are followed by periods of partial or complete recovery, known as remissions. During remission, symptoms may disappear completely, although some degree of permanent damage to nerves often occurs.
RMS is the most common initial diagnosis among individuals with MS, accounting for approximately 85% of cases. Understanding its nature is essential for timely intervention and effective management.
Symptoms of Relapsing Form of Multiple Sclerosis
Symptoms of RMS vary widely depending on the location and extent of nerve damage. Common symptoms include:
- Visual disturbances: blurred vision, double vision, or loss of vision
- Motor symptoms: muscle weakness, spasticity, and coordination issues
- Sensory problems: numbness, tingling sensations, or chronic pain
- Cognitive impairment: memory loss, attention difficulties, and slowed information processing
- Fatigue: severe, disabling tiredness that is unrelated to activity levels
- Bladder and bowel dysfunction: urgency, frequency, and incontinence issues
- Emotional changes: depression, anxiety, and mood swings
The severity and duration of symptoms can differ between individuals and episodes, making RMS highly unpredictable.
Causes and Risk Factors of RMS
The exact cause of RMS remains unknown, but several factors are believed to contribute:
- Autoimmune Dysfunction: The immune system attacks the central nervous system, damaging the myelin sheath that protects nerve fibers.
- Genetics: A family history of MS increases susceptibility.
- Environmental Factors: Low vitamin D levels, smoking, and viral infections such as Epstein-Barr virus may trigger MS.
- Age and Gender: RMS typically manifests between ages 20 and 40 and affects women more than men.
These risk factors collectively influence the likelihood of developing RMS but do not guarantee disease onset.
How Is RMS Diagnosed?
A diagnosis of RMS requires a careful evaluation by a neurologist, involving:
- Magnetic Resonance Imaging (MRI): Detects areas of demyelination (lesions) in the brain and spinal cord.
- Lumbar Puncture: Analyzes cerebrospinal fluid for specific antibodies associated with MS.
- Evoked Potentials: Measures the speed of nerve signals, helping to identify damaged pathways.
- Clinical History: Documented evidence of attacks separated in time and space (different parts of the nervous system) is essential.
Early and accurate diagnosis enables prompt initiation of disease-modifying therapies (DMTs), which can significantly impact disease progression.
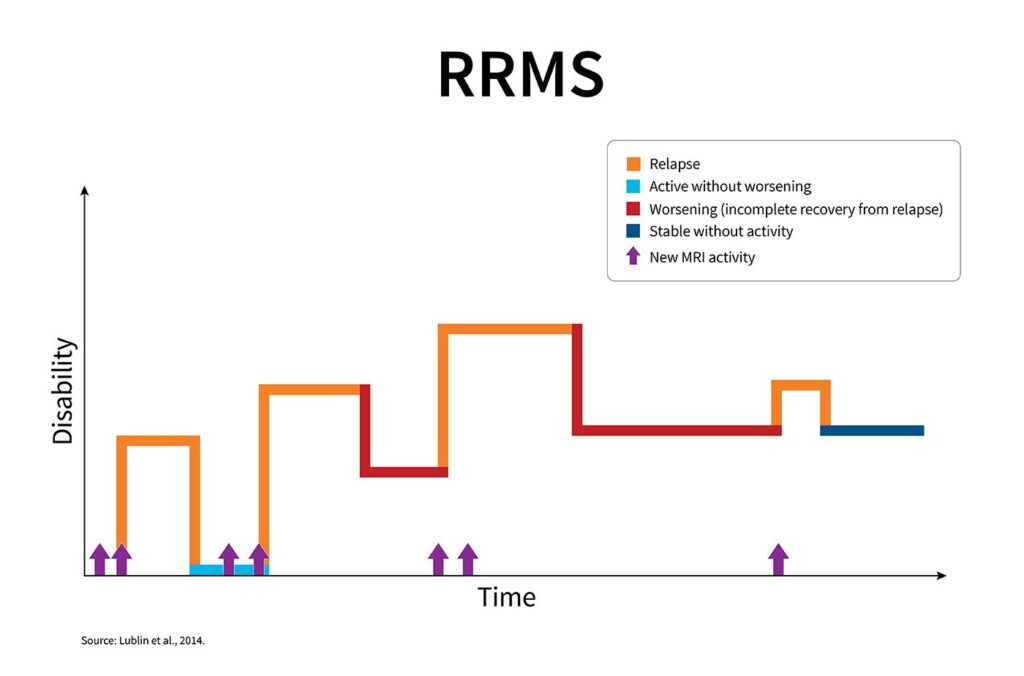
Disease Progression: From RMS to Secondary Progressive MS
Over time, many individuals with RMS transition to Secondary Progressive Multiple Sclerosis (SPMS). In SPMS, the disease shifts from relapsing-remitting episodes to a gradual worsening of neurologic function independent of relapses.
Mermaid Diagram:
Understanding this progression is crucial for selecting appropriate long-term management strategies.
Treatment Options for Relapsing Form of Multiple Sclerosis
1. Disease-Modifying Therapies (DMTs)
DMTs reduce the frequency and severity of relapses, delay progression, and limit new lesion formation. Common DMTs include:
- Injectables: Interferon beta-1a, Glatiramer acetate
- Oral Medications: Dimethyl fumarate, Fingolimod, Teriflunomide
- Infusions: Natalizumab, Ocrelizumab, Alemtuzumab
Each therapy has unique efficacy rates and risk profiles, necessitating a tailored approach based on individual needs and preferences.
2. Relapse Management
High-dose corticosteroids such as methylprednisolone are typically administered during acute relapses to shorten the duration and severity of symptoms.
3. Symptom Management
Pharmacologic and non-pharmacologic treatments address specific symptoms like spasticity, fatigue, pain, and bladder dysfunction. Physical therapy, occupational therapy, and psychological counseling further enhance quality of life.
Lifestyle Modifications to Support RMS Management
Optimal management of RMS extends beyond pharmacological interventions:
- Balanced Diet: Anti-inflammatory diets rich in fruits, vegetables, and omega-3 fatty acids may be beneficial.
- Exercise: Regular, moderate exercise improves strength, mobility, and mental health.
- Stress Reduction: Techniques such as mindfulness meditation and yoga can mitigate stress-related exacerbations.
- Avoiding Smoking: Smoking cessation is critical, as it accelerates MS progression.
Adopting a healthy lifestyle complements medical treatment and improves overall prognosis.
Latest Research and Future Directions
Ongoing research in RMS focuses on:
- Biomarker Discovery: Identifying biological indicators for early diagnosis and personalized treatment.
- Remyelination Therapies: Investigating agents that promote repair of damaged myelin.
- Neuroprotective Agents: Developing drugs aimed at preserving nerve fibers and preventing irreversible damage.
The future holds promising advances that could revolutionize the care and outcomes for individuals with RMS.
Frequently Asked Questions:
What distinguishes RMS from progressive forms of MS?
RMS is marked by distinct relapse and remission phases, while progressive forms of MS involve continuous neurological decline without remission periods.
Can RMS be cured?
There is currently no cure for RMS, but early treatment with DMTs and lifestyle changes can significantly reduce disease activity and delay progression.
How long do remissions last in RMS?
Remissions can last weeks, months, or even years. Their duration and completeness vary widely among individuals.
Are there alternative treatments for RMS?
Complementary therapies like acupuncture, massage, and herbal supplements may offer symptom relief but should not replace conventional medical treatments.
How does pregnancy affect RMS?
Pregnancy often reduces relapse rates, particularly in the third trimester. However, relapse risk can increase postpartum, necessitating careful planning with healthcare providers.