Chronic lymphocytic leukemia (CLL) is a type of cancer that originates in the blood and bone marrow, characterized by the uncontrolled growth of B lymphocytes (a type of white blood cell). Though CLL is often indolent and progresses slowly, patients may experience relapse after a period of remission. A relapsed CLL is defined as the return of the disease after initial treatment, and managing this form of leukemia presents a unique challenge for both clinicians and patients.
In this comprehensive article, we explore the causes, symptoms, treatment options, and prognosis for relapsed chronic lymphocytic leukemia, offering insights into modern therapeutic approaches and survival outcomes.
What Is Relapsed Chronic Lymphocytic Leukemia?
Definition of Relapsed CLL
Relapsed CLL occurs when the disease, which was previously under control or in remission, begins to worsen again after a period of treatment response. This can happen after months or years of remission, presenting a major obstacle in the ongoing treatment of the disease. A relapse typically indicates that the leukemia cells have evolved or become resistant to prior therapies, necessitating a reevaluation of treatment strategies.
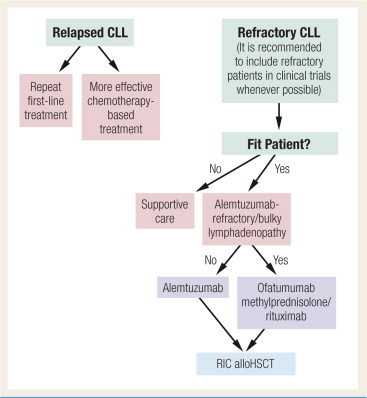
Differentiating Relapsed and Refractory CLL
While both terms refer to a lack of response to treatment, “refractory CLL” refers to a disease that does not respond to treatment from the outset, whereas “relapsed CLL” denotes a recurrence after an initial response. Understanding the nuances between these two conditions is vital for appropriate treatment planning.
Causes and Risk Factors of Relapsed Chronic Lymphocytic Leukemia
Genetic and Molecular Factors
The relapse of CLL is often linked to genetic mutations and molecular changes in the leukemia cells. Mutations in genes like TP53 (which controls cell division and apoptosis) and IGHV (Immunoglobulin heavy chain variable region) can lead to increased resistance to treatment. These mutations can render the leukemia cells more aggressive and less responsive to conventional therapies, leading to relapse.
Minimal Residual Disease (MRD)
One of the main reasons for relapse is the presence of minimal residual disease (MRD) following treatment. MRD refers to a small number of leukemia cells that remain in the body after therapy, which can later proliferate and cause the disease to return. Detecting MRD through advanced imaging and molecular techniques can help predict the likelihood of relapse and tailor treatment plans accordingly.
Prior Treatments and Disease Stage
The stage of CLL at the time of diagnosis and the treatments used during the initial therapy also play a significant role in determining the likelihood of relapse. Patients who undergo chemotherapy alone without additional targeted therapies may have a higher chance of relapse. Additionally, patients diagnosed at a later stage of the disease, when leukemia cells are more widespread, may be more susceptible to relapse.
Symptoms of Relapsed Chronic Lymphocytic Leukemia
The symptoms of relapsed CLL often resemble those experienced during the initial stages of the disease, but they may present more aggressively.
Common Symptoms of Relapsed CLL:
- Swollen lymph nodes: Particularly in the neck, armpits, or groin, lymph node enlargement is a hallmark symptom.
- Fatigue: A feeling of exhaustion and weakness that persists despite rest, often indicating disease progression.
- Unexplained weight loss: Weight loss without any intentional change in diet or activity levels.
- Fever and night sweats: These “B symptoms” are common in lymphoproliferative diseases like CLL.
- Pain or discomfort: Discomfort in the chest, abdomen, or bones due to the spread of the disease.
Patients may also experience frequent infections, bruising, or prolonged bleeding due to the impaired immune system and platelet counts, which are characteristic of relapsed CLL.
Treatment Options for Relapsed Chronic Lymphocytic Leukemia
Treating relapsed CLL requires a comprehensive approach that takes into account the patient’s previous treatments, disease characteristics, and overall health. With advancements in cancer therapies, numerous treatment modalities are now available.
Targeted Therapy
Targeted therapy is often the first line of defense in treating relapsed CLL. These therapies focus on specific proteins or genetic mutations that drive the cancer’s growth. Unlike traditional chemotherapy, targeted treatments generally have fewer side effects.
Examples of Targeted Therapies for CLL:
- Bruton’s Tyrosine Kinase (BTK) Inhibitors: Drugs like Ibrutinib and Acalbrutinib block signals that help CLL cells grow and survive, showing significant efficacy in relapsed cases.
- BCL-2 Inhibitors: Venetoclax is an example of a BCL-2 inhibitor that targets proteins responsible for preventing cancer cell death, promoting CLL cell apoptosis.
- PI3K Inhibitors: Drugs like Idelalisib interfere with the PI3K signaling pathway, which is crucial for CLL cell survival.
Immunotherapy
Immunotherapy is increasingly being used in the treatment of relapsed CLL, aiming to enhance the body’s immune response to fight cancer cells. Monoclonal antibodies, such as Rituximab, target the CD20 protein on CLL cells, marking them for destruction by the immune system. When used in combination with chemotherapy or other therapies, monoclonal antibodies can significantly improve outcomes.
CAR T-cell Therapy is another promising form of immunotherapy. In this approach, a patient’s T-cells are engineered to recognize and attack leukemia cells, offering hope for those with refractory or relapsed CLL.
Chemotherapy
Chemotherapy, although not the first-line treatment for relapsed CLL, may still be considered for patients with aggressive disease or those who do not respond to targeted therapies. Regimens such as FCR (Fludarabine, Cyclophosphamide, and Rituximab) have been used in relapsed settings with varying success, although the side effects can be significant.
Stem Cell Transplantation
For some patients with high-risk relapsed CLL, allogeneic stem cell transplantation may be an option. This treatment involves replacing the patient’s diseased bone marrow with healthy stem cells from a donor. While it offers the potential for a cure, stem cell transplantation is associated with a high risk of complications, including graft-versus-host disease.
Clinical Trials
Patients with relapsed CLL may also be candidates for clinical trials that investigate novel therapies, including new drug combinations, immunotherapy approaches, and cellular therapies. Participating in a clinical trial can provide access to cutting-edge treatments that are not yet widely available.
Prognosis for Relapsed Chronic Lymphocytic Leukemia
The prognosis for relapsed CLL depends on several factors, including the patient’s age, overall health, genetic markers, and response to prior therapies. While relapsed CLL is generally considered a challenging condition to treat, advances in targeted therapies and immunotherapy have significantly improved outcomes in recent years.
Factors Affecting Prognosis:
- Genetic mutations: The presence of mutations like TP53 can worsen prognosis, as these mutations make the disease more resistant to treatment.
- Treatment response: How well a patient responds to first-line therapies influences long-term survival outcomes. Those who relapse early may have a more guarded prognosis.
- Age and general health: Younger patients in good health generally have better survival rates and are more likely to tolerate aggressive treatments.
Recent advances in treatment options, such as BTK inhibitors and CAR T-cell therapy, have significantly improved the outlook for patients with relapsed CLL. However, long-term remission remains difficult to achieve for some, and ongoing research continues to explore new therapies that could offer better outcomes.
Relapsed chronic lymphocytic leukemia presents unique challenges in treatment, requiring a personalized approach that includes targeted therapies, immunotherapy, and potentially stem cell transplantation. The advancements in treatment options, particularly with the advent of newer drugs and therapies, offer hope for those with relapsed or refractory CLL. While the prognosis can be challenging, the future of CLL treatment is promising, and ongoing research holds the potential to further improve outcomes for patients affected by this persistent form of leukemia.

