Recurrent vulvovaginal candidiasis (RVVC) is defined as four or more documented episodes of symptomatic vulvovaginal candidiasis within a 12-month period. It affects millions of women globally, significantly impacting quality of life and posing substantial management challenges due to its recurrent nature.
Causes and Risk Factors of Recurrent Vulvovaginal Candidiasis
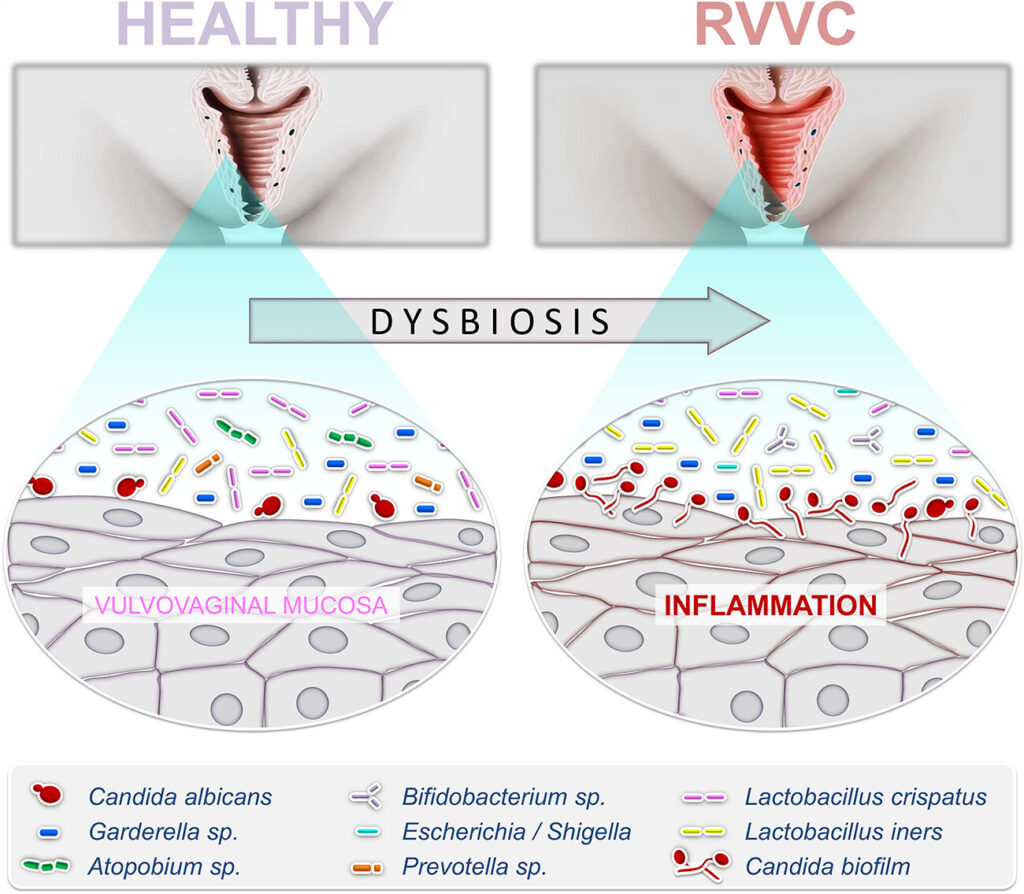
The pathogenesis of RVVC involves a complex interplay between host factors, microbial virulence, and environmental influences:
- Candida Species: Candida albicans accounts for most cases, though non-albicans species like C. glabrata are increasingly implicated.
- Immunologic Factors: Impaired local immune responses, particularly in innate immunity and Th17 pathways.
- Antibiotic Use: Disruption of normal vaginal flora predisposes to Candida overgrowth.
- Hormonal Influences: Elevated estrogen levels during pregnancy, contraceptive use, or hormone replacement therapy.
- Diabetes Mellitus: Poor glycemic control enhances fungal proliferation.
- Genetic Susceptibility: Variations in genes related to pattern recognition receptors and cytokine production.
Pathophysiology of Recurrent Vulvovaginal Candidiasis
The pathophysiological cycle of RVVC can be visualized as follows:
Failure to eliminate colonizing Candida strains or altered host defense mechanisms sustains this vicious cycle of relapse.
Clinical Presentation of Recurrent Vulvovaginal Candidiasis
Patients with RVVC often exhibit consistent symptoms with each episode:
- Vaginal Itching and Burning: Intense discomfort affecting daily activities.
- Thick, White Vaginal Discharge: Classically described as “cottage cheese-like” without significant odor.
- Vulvar Erythema and Edema: Redness, swelling, and sometimes excoriations due to scratching.
- Dysuria and Dyspareunia: Pain during urination and sexual intercourse.
Symptoms tend to worsen premenstrually and during periods of high estrogen exposure.
Diagnostic Evaluation for Recurrent Vulvovaginal Candidiasis
Accurate diagnosis of RVVC requires confirmation of Candida infection through:
- Microscopic Examination: Detection of budding yeast and pseudohyphae in wet mount or KOH preparation.
- Culture: Fungal culture to identify Candida species, especially if standard therapy fails.
- Molecular Testing: PCR assays can detect mixed infections and non-albicans Candida.
- Assessment of Predisposing Factors: Blood glucose evaluation, hormonal status, and medication history review.
Distinguishing RVVC from other causes of vulvovaginitis such as bacterial vaginosis and trichomoniasis is essential for appropriate management.
Treatment Strategies for Recurrent Vulvovaginal Candidiasis
Induction Therapy
- Oral Fluconazole: 150 mg every 72 hours for three doses is the standard induction regimen.
- Topical Azoles: Clotrimazole, miconazole, or terconazole applied intravaginally for 7–14 days.
Maintenance Therapy
- Oral Fluconazole: 150 mg weekly for six months post-induction reduces relapse rates dramatically.
- Alternative Maintenance Options: Topical therapy for fluconazole-resistant strains or azole-refractory cases.
Management of Non-Albicans Candida
- Boric Acid Suppositories: 600 mg intravaginally daily for 14 days followed by maintenance if necessary.
- Nystatin Suppositories: Particularly useful for Candida glabrata infections.
Emerging Therapies and Future Directions
Recent advancements offer promising alternatives for RVVC management:
- Oteseconazole: A novel azole with enhanced activity against azole-resistant Candida strains.
- Immunotherapy: Vaccines targeting Candida cell wall components are under investigation.
- Probiotic Supplementation: Restoration of normal vaginal flora with Lactobacillus strains to prevent recolonization.
Prevention of Recurrent Vulvovaginal Candidiasis
Effective preventive strategies include:
- Glycemic Control: Tight diabetes management.
- Probiotic Use: Regular use of oral or vaginal probiotics.
- Avoiding Unnecessary Antibiotics: Rational antibiotic prescribing practices.
- Lifestyle Adjustments: Wearing breathable cotton underwear, avoiding douches, and maintaining good genital hygiene.
Patient education plays a critical role in minimizing triggers and promoting adherence to preventive regimens.
Complications of Recurrent Vulvovaginal Candidiasis
RVVC, if poorly managed, can lead to:
- Chronic Vulvar Pain Syndromes: Including vulvodynia and vestibulitis.
- Psychological Impact: Anxiety, depression, and sexual dysfunction due to persistent symptoms.
- Antifungal Resistance: Resulting from overuse or inappropriate use of antifungal agents.
Early intervention and tailored therapy are key to mitigating these risks.
Prognosis for Women with Recurrent Vulvovaginal Candidiasis
With appropriate induction, maintenance, and preventive strategies, most women achieve symptom control and long-term remission. Nevertheless, vigilance is required, as underlying predispositions can cause occasional relapses even after successful initial therapy.
Recurrent vulvovaginal candidiasis is a multifactorial condition requiring a comprehensive, individualized approach. By combining optimal antifungal therapy, addressing host predisposing factors, and implementing preventive measures, we can significantly improve outcomes for affected women. Ongoing research into novel therapies and vaccines holds promise for transforming the future management of RVVC.